Complications of diabetes: a threat to life
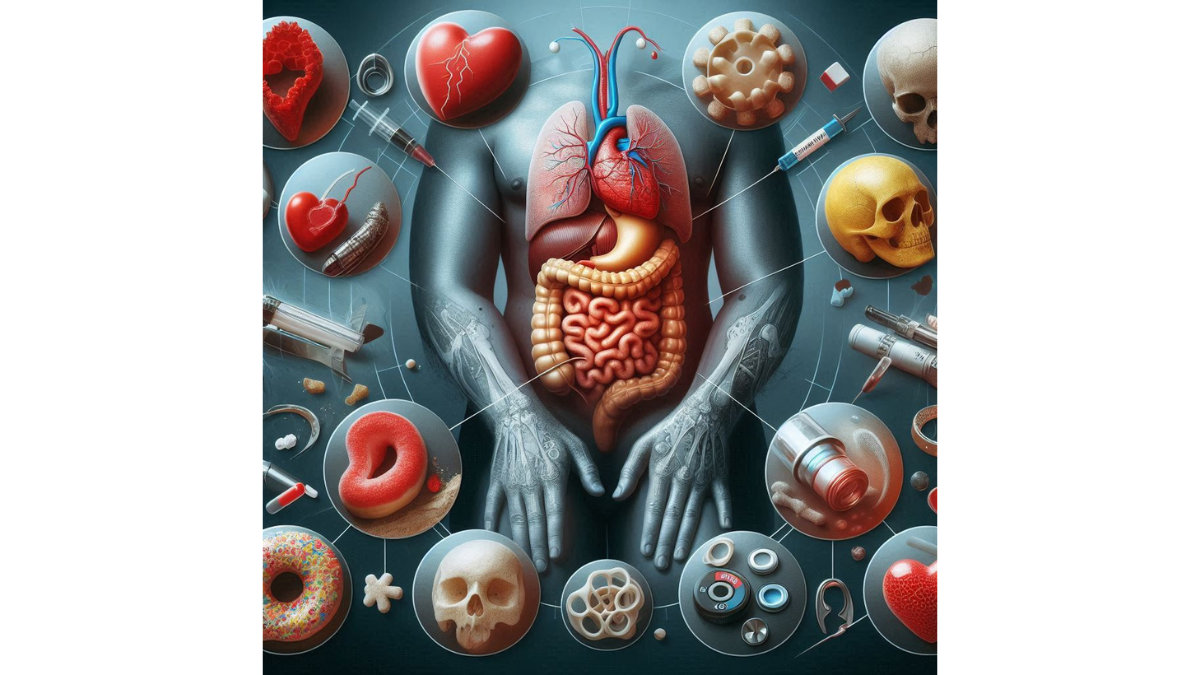
Complications of diabetes: a threat to life – Diabetes is more than just a condition that affects your blood sugar levels; it’s a complex, multifaceted disease that requires careful management to avoid serious health issues in the long run. When you have diabetes, your body either doesn’t produce enough insulin or is unable to use it effectively. Insulin is crucial because it helps regulate your blood sugar levels, and when these levels remain consistently high, it can lead to various complications. Imagine managing diabetes like maintaining a balanced ecosystem. When everything is in harmony, all the elements function well together. However, neglecting one component can lead to a cascade of problems. This analogy underlines the importance of monitoring your condition closely and making informed lifestyle choices.
Types of Diabetes Complications
Diabetes complications can be broadly categorized into two main groups: microvascular and macrovascular complications.
Microvascular Complications
These involve damage to small blood vessels and include:
- Diabetic Retinopathy: Damage to the blood vessels in the retina, potentially leading to blindness.
- Diabetic Nephropathy: Kidney damage that can progress to kidney failure.
- Diabetic Neuropathy: Nerve damage, often leading to pain and loss of sensation.
Macrovascular Complications
These involve damage to large blood vessels, resulting in:
- Heart Disease: Increased risk of heart attacks due to stiffening arteries.
- Stroke Risk: Elevated risk of stroke, which can impact mobility and cognitive function.
Each of these complications can significantly affect your quality of life, highlighting the importance of proactive diabetes management. If you think of your diabetic journey like a race, recognizing the risks and preparing for them is essential to cross the finish line successfully. By understanding both the disease and its potential complications, you can take informed steps to minimize risks and enhance your well-being.
Cardiovascular Complications
Heart Disease
As you navigate the complexities of managing diabetes, it’s crucial to be aware of its impact on your heart health. Heart disease is one of the most common complications associated with diabetes. It’s alarming to know that people with diabetes are twice as likely to develop heart disease compared to those without the condition. Think of your heart as the engine that drives your body’s performance. With diabetes, the engine can become strained due to high blood sugar levels, leading to atherosclerosis, where arteries become clogged and less flexible. This can result in:
- Heart Attack: blocked blood flow to the heart muscle.
- Coronary artery disease: leading to chest pain (angina) or heart failure.
- High Blood Pressure: which can further damage your blood vessels.
Lifestyle choices play a pivotal role here. Incorporating heart-healthy foods like fruits, vegetables, whole grains, and lean proteins can positively impact your cardiovascular health. Regular exercise and weight management are equally important in reducing these risks.
Stroke Risk
In addition to heart disease, managing diabetes effectively can significantly reduce your stroke risk. Diabetes can damage large blood vessels, and this correlates directly with an increased likelihood of stroke. In fact, research shows that individuals with diabetes are nearly two to four times more likely to experience a stroke. A stroke occurs when blood flow to the brain is disrupted, which can lead to long-term disabilities or even death. Here are some risk factors to keep in mind:
- High Blood Sugar Levels: Higher than normal levels can damage blood vessels over time.
- Hypertension: Often accompanies diabetes and exacerbates the risk of strokes.
- High Cholesterol: Can result from poor dietary choices, further aggravating blood flow issues.
To reduce the risk of stroke, consider the following actions:
- Maintain consistent blood sugar levels through medication and diet.
- Monitor blood pressure and cholesterol levels regularly.
- Engage in regular physical activities like walking, swimming, or cycling.
By being proactive and adjusting your lifestyle, you can help shield your heart and brain from the devastating effects of diabetes-related cardiovascular complications. Just remember, the small changes you make today can lead to significant health benefits in the years to come.
Neurological Complications
Diabetic Neuropathy
One of the more challenging aspects of living with diabetes is the risk of developing diabetic neuropathy, a condition that arises from prolonged high blood sugar levels damaging the nerves. Imagine feeling a persistent tingling, numbness, or pain in your feet or hands—these are hallmarks of neuropathy that many individuals with diabetes face daily. Diabetic neuropathy typically manifests in four types:
- Peripheral Neuropathy: Affects the feet and hands, often leading to pain and loss of sensation.
- Autonomic Neuropathy: Impacts the nerves that control internal organs, causing issues like digestive problems or sweating abnormalities.
- Proximal Neuropathy: Affects the hips, thighs, or buttocks, leading to weakness and pain in those areas.
- Focal Neuropathy: Impacts specific nerves, often resulting in sudden weakness or pain, frequently in the eyes or torso.
It’s crucial to recognize these symptoms early. Many people may dismiss tingling sensations as temporary discomfort, but being proactive and discussing these changes with your healthcare provider can lead to effective management strategies. Simple lifestyle changes—like regular foot exams and proper footwear—can help prevent further complications.
Cognitive Impairment
Beyond physical symptoms, diabetes can also affect cognitive function. Cognitive impairment is a growing concern in the diabetes community, with studies suggesting that high blood sugar levels may contribute to issues like memory loss and difficulty concentrating. Imagine sitting down to read a book but struggling to remember the details just moments later; that’s what cognitive impairment may feel like. It’s a worrying reality for many, and here are some risk factors to consider:
- Chronic High Blood Sugar: Ongoing hyperglycemia can lead to inflammation and damage in the brain.
- Age: Older adults with diabetes are particularly at risk for cognitive decline.
- Comorbid Conditions: Issues like heart disease can increase the likelihood of cognitive problems.
To support cognitive health, consider these strategies:
- Engage in regular mental exercises, such as puzzles or reading.
- Maintain a balanced diet rich in omega-3 fatty acids, antioxidants, and vitamins that support brain health.
- Stay socially active by participating in group activities or conversations—stimulation from interactions can bolster cognitive function.
Managing diabetes is not just about controlling blood sugar levels—it’s also about safeguarding your overall neurological health. By being vigilant and proactive, you can significantly mitigate these risks and maintain a better quality of life.
Kidney Complications
Diabetic Nephropathy
As you delve deeper into the impact of diabetes, it becomes essential to recognize its effect on kidney health, particularly through a condition known as diabetic nephropathy. This complication occurs when high blood sugar levels slowly damage the kidneys’ filtering units, leading to increased protein in the urine—a sign that something is amiss. Diabetic nephropathy doesn’t usually present symptoms until it has progressed significantly, making regular check-ups crucial. Here are some key points to keep in mind regarding this condition:
- Early Warning Signs: Look out for slight changes in urine, such as foamy urine, which can indicate protein presence.
- Risk Factors: Factors like uncontrolled blood sugar, high blood pressure, and a family history of kidney disease contribute significantly to the risk of developing nephropathy.
- Prevention: Staying on top of your diabetes management plan, including blood glucose control and maintaining healthy blood pressure levels, can dramatically reduce your risk.
Regular screening is vital. As someone managing diabetes, asking your doctor about urine tests and kidney function evaluations can help catch any issues early.
Renal Failure
If diabetic nephropathy goes untreated, it may progress to a more severe stage known as renal failure. Renal failure occurs when the kidneys can no longer effectively filter waste products from your blood, leading to a buildup of toxins in your body—a situation that can be life-threatening. Imagine feeling increasingly fatigued, dealing with swelling in your legs or feet, or experiencing persistent nausea. These may be indications of renal failure. Here are a few crucial aspects to think about:
- Types of Renal Failure: It can be acute or chronic. Acute renal failure can develop quickly, while chronic renal failure progresses over time, often requiring intensive management.
- Symptoms to Monitor: Key symptoms include reduced urine output, unexplained weight loss, or confusion.
- Treatment Options: If it advances to end-stage renal failure, options include dialysis or a kidney transplant—both of which carry significant lifestyle changes and medical considerations.
To protect your kidney health, remember the importance of regular check-ups, maintaining a balanced diet low in processed foods, and staying hydrated. Additionally, incorporating foods rich in antioxidants, like berries and leafy greens, may help, as these can combat oxidative stress in the kidneys. By prioritizing your kidney health, you can take essential steps to prevent nephropathy and its potential progression to renal failure, ensuring a more complete understanding of how diabetes affects your body.
Eye Complications
Diabetic Retinopathy
When it comes to diabetes, the repercussions extend beyond the physical body; they can significantly impact your vision as well. One of the most serious eye complications is diabetic retinopathy, a condition that affects the retina, the light-sensitive tissue at the back of your eye. Imagine trying to read a favorite book but struggling to see the words clearly. This inability to see isn’t just an inconvenience; it can be a sign of diabetic retinopathy. The condition develops when high blood sugar levels damage the tiny blood vessels in the retina, leading to:
- Early Symptoms: Often, there are no early symptoms, which is why regular eye exams are critical. Some might notice blurred vision or difficulty seeing at night.
- Progressive Stages: Diabetic retinopathy progresses from mild nonproliferative to severe proliferative stages, where new blood vessels form and can bleed into the eye.
- Risk Factors: Consistently high blood sugar levels, duration of diabetes, and high blood pressure can elevate your risk.
Routine eye examinations can catch these changes early, allowing for timely treatment options like laser therapy or injections that can slow or even halt the progression of the disease.
Glaucoma and Cataracts
In addition to diabetic retinopathy, individuals with diabetes are also at a heightened risk for other eye complications such as glaucoma and cataracts. It’s essential to understand how these conditions can affect your vision over time.
- Glaucoma: This condition causes fluid buildup in the eye, leading to increased pressure and potential damage to the optic nerve. Early detection is key, as it often progresses without symptoms. Regular screenings can help detect it early, allowing for treatments to manage the intraocular pressure effectively.
- Cataracts: People with diabetes are more likely to develop cataracts, which cause the lens of the eye to cloud, leading to blurred vision. This can feel like looking through a frosted window. Surgical intervention is a common and effective treatment for cataracts, restoring clear vision in many instances.
To safeguard your eyesight, consider these proactive measures:
- Schedule regular comprehensive eye exams—don’t wait for symptoms to develop.
- Control your blood sugar levels, as managing diabetes is crucial to reducing the risk of eye complications.
- Maintain a healthy diet rich in antioxidants, which can benefit eye health, such as leafy greens and colorful fruits.
By staying vigilant about your eye health, you can effectively minimize the risks of diabetic retinopathy, glaucoma, and cataracts, ensuring better overall vision and quality of life as you manage your diabetes.
Skin Complications
Diabetic Dermopathy
As you continue to explore the effects of diabetes on your body, it becomes evident that skin complications can also arise, one of which is diabetic dermopathy. Often overlooked, this condition presents as light brown, scaly patches, typically found on the lower legs. While it might not be painful, it can serve as a visible reminder of the underlying issues related to diabetes management. When I first noticed a few spots developing on my skin, I was puzzled but didn’t think much of it. However, learning about diabetic dermopathy helped me realize the importance of paying attention to skin changes, as they could signal fluctuations in blood sugar levels. Key points to consider about diabetic dermopathy include:
- Causes: Poor blood circulation and nerve damage linked to diabetes contribute to these changes in your skin.
- Symptoms: You’ll often notice these spots appearing without any accompanying pain or itching, making them easy to dismiss.
- Management: While diabetic dermopathy usually doesn’t require treatment, keeping your blood sugar levels stable can help prevent new spots from forming.
Fungal Infections
In addition to diabetic dermopathy, individuals with diabetes are also more prone to fungal infections. High sugar levels in the blood create an environment conducive to these infections, particularly around warm and moist areas of the body like:
- Feet: Athletes’ foot can occur when moisture is trapped, leading to itching and discomfort.
- Groin Area: Yeast infections may develop and cause irritation and a rash.
- Nails: Fungal nail infections can lead to discoloration and brittleness.
Here are some helpful tips to minimize the risk of these infections:
- Maintain Hygiene: Regularly wash and dry the areas prone to moisture.
- Choose Breathable Fabrics: Wearing loose-fitting cotton clothing can help keep these areas dry and reduce infection risk.
- Monitor Your Feet: Pay special attention to any cracks, cuts, or areas of irritation, as these can invite infections.
By being proactive in monitoring skin changes and practicing good hygiene, you can effectively manage the risks associated with diabetic skin complications. Remember, your skin is a reflection of your overall health, and staying vigilant about changes can prevent more serious complications down the line.
Foot Complications
Diabetic Foot Ulcers
One of the more serious complications of diabetes is the development of diabetic foot ulcers, which can be particularly concerning considering the potential for severe consequences. Picture this: you’ve noticed a small sore on your foot, and it doesn’t seem to heal. For someone with diabetes, that seemingly innocuous sore can quickly escalate into a diabetic foot ulcer, which is an open wound that can become infected. Diabetic foot ulcers develop as a result of various factors, including:
- Reduced Blood Flow: High blood sugar levels can damage blood vessels, reducing blood supply to the feet.
- Neuropathy: Loss of sensation in the feet may lead to unnoticed injuries.
- Increased Pressure: Ill-fitting shoes or foot deformities can place undue pressure on certain areas.
I remember a friend who had to deal with a foot ulcer; the initial irritation turned into a significant health concern. The healing process was long and complicated, reinforcing the need for vigilant foot care. To minimize your risk of developing foot ulcers, consider the following tips:
- Regular Foot Checks: Inspect your feet daily for any cuts, blisters, or changes in color.
- Proper Footwear: Choose shoes that fit well and provide adequate support, and avoid walking barefoot.
- Maintain Hygiene: Keep your feet clean and dry, and moisturize to prevent cracking.
Peripheral Arterial Disease
In addition to diabetic foot ulcers, another complication that can significantly affect foot health is peripheral arterial disease (PAD). This condition arises when the blood vessels that supply blood to the legs and feet become narrowed or blocked due to atherosclerosis. With PAD, you might experience symptoms such as:
- Leg Pain: Discomfort when walking or climbing stairs due to reduced blood flow.
- Coldness in the Foot: A noticeable difference in temperature between your feet and legs.
- Wounds That Heal Slowly: Similar to foot ulcers, slow-healing wounds can be an indicator of compromised blood flow.
To combat PAD and protect your foot health, consider these strategies:
- Regular Exercise: Engaging in moderate physical activity can help improve circulation.
- Quit Smoking: If you smoke, quitting can significantly reduce your risk of PAD and improve overall blood flow.
- Healthy Diet: Consume a balanced diet rich in fruits, vegetables, and whole grains while minimizing saturated fats.
Recognizing the importance of foot health in diabetes management can not only prevent complications but also enhance your quality of life. By being proactive and maintaining a consistent foot care routine, you can protect your feet, allowing you to move with confidence and comfort.
Dental Complications
Gum Disease
As you continue your journey through the effects of diabetes on your overall health, dental complications are an essential aspect to address, starting with gum disease. This condition often sneaks up on individuals, yet it can have significant consequences not only for oral health but also for your systemic well-being. Gum disease, also known as periodontal disease, manifests in two stages:
- Gingivitis: The early stage characterized by red, swollen gums that may bleed during brushing or flossing.
- Periodontitis: A more advanced stage where gums begin to pull away from the teeth, leading to bone loss and the potential for tooth loss.
Many people don’t realize that individuals with diabetes are more prone to gum disease due to high blood sugar levels that can impair blood flow and inflammation. I once had a colleague who was surprised to learn about the link between her diabetes and her persistent gum issues. She struggled with chronic gingivitis, which eventually led her to make dental health a priority. To maintain healthy gums, consider these proactive measures:
- Regular Dental Check-ups: Schedule visits every six months or as recommended by your dentist to keep tabs on your oral health.
- Daily Oral Hygiene: Brush twice daily and floss at least once to remove plaque and prevent tartar buildup.
- Healthy Lifestyle Choices: Monitor your blood sugar levels and maintain a balanced diet low in sugary foods, which can exacerbate gum disease.
Tooth Loss
If gum disease is not managed, it can lead to tooth loss, which can be both physically and emotionally challenging. Losing teeth can significantly impact your ability to eat, speak, and even smile confidently. Tooth loss due to periodontal disease often unfolds as follows:
- Increased Mobility: As the supporting structures weaken, your teeth may become loose and shift.
- Pain and Discomfort: Damaged gums can lead to soreness, making it difficult to chew or consume certain foods.
- Aesthetic Concerns: Missing teeth can alter your facial structure and negatively impact your self-esteem.
Taking care of your teeth and gums is crucial to preventing tooth loss in diabetes. Here are some tips to minimize the risk:
- Use an Antimicrobial Mouthwash: Rinsing with an antimicrobial mouthwash can help reduce plaque and maintain gum health.
- Stay Hydrated: Drinking plenty of water helps wash away food particles and supports saliva production, which plays a role in oral health.
- Consider Professional Cleanings: Regular dental cleanings can effectively manage plaque buildup and keep your gums healthy.
Incorporating these practices into your routine can go a long way in managing dental complications associated with diabetes. Remember, your oral health is an integral part of your overall well-being, and by prioritizing it, you can enhance both your comfort and confidence.
Sexual Complications
Erectile Dysfunction
As you navigate the overarching impact of diabetes on your health, it’s essential to touch upon sexual complications, particularly erectile dysfunction (ED). This condition can be a sensitive topic, but it’s crucial to understand that it’s not uncommon for men with diabetes. Erectile dysfunction occurs when blood flow to the penis is restricted or when nerve signals that trigger an erection are damaged. Research indicates that men with diabetes are at least three times more likely to experience ED. I recall a conversation with an acquaintance who felt embarrassed discussing his struggles but later found relief in knowing he was not alone and that treatment options were available. Factors contributing to ED in diabetes can include:
- Poor Blood Sugar Control: Elevated glucose levels can damage the blood vessels and nerves that are vital for achieving an erection.
- Psychological Factors: Anxiety and depression, which can accompany chronic diseases, may also contribute.
- Peripheral Neuropathy: Nerve damage can decrease sensation, impacting sexual performance.
Fortunately, a range of treatment options exists, from medications like PDE5 inhibitors to lifestyle changes such as weight management and quitting smoking. Open communication with your healthcare provider can also help personalize solutions tailored to your needs.
Low Libido
In addition to erectile dysfunction, low libido is another sexual complication often reported by individuals with diabetes. This decrease in sexual desire can stem from various physical and emotional factors linked to diabetes management. For many, low libido may arise due to:
- Hormonal Changes: Fluctuations in testosterone levels can reduce sexual interest.
- Chronic Fatigue: Managing diabetes can be tiring, both physically and mentally, potentially impacting your desire.
- Emotional Stress: Feelings of frustration or anxiety regarding health can diminish libido.
Open discussions about sexual health are vital. I remember a friend mentioning how much lighter she felt after bringing her concerns about low libido to her doctor. They explored her options together, leading to improved strategies for managing stress and enhancing connection with her partner. To foster a healthy sexual desire, consider these tips:
- Prioritize Self-Care: Focus on proper diabetes management, including blood sugar control, healthy eating, and regular exercise.
- Communicate Openly: Talk with your partner about your feelings and needs; a strong emotional connection can bolster libido.
- Seek Professional Help: Don’t hesitate to consult with your healthcare provider for personalized advice and treatment options to address both erectile dysfunction and low libido effectively.
Navigating sexual health in the context of diabetes can seem daunting, but being informed and proactive can significantly improve your quality of life and intimate relationships.
Mental Health Complications
Depression
As you explore the multifaceted nature of living with diabetes, it’s crucial to acknowledge the significant impact it can have on mental health. One of the most prevalent mental health complications is depression. Living with a chronic condition like diabetes can bring about feelings of sadness, hopelessness, and fatigue. I remember hearing my friend express, “Sometimes it just feels overwhelming to manage my diabetes on top of everything else in life.” This sentiment resonates with many people facing similar challenges. Research indicates that individuals with diabetes are at a higher risk of developing depression, which can, in turn, affect their ability to manage their condition effectively. Here are some key factors to be aware of:
- Emotional Weight: The constant adjustments in lifestyle, dietary choices, and medication management can take an emotional toll.
- Physical Symptoms: Symptoms of depression can overlap with diabetes-related fatigue, making it difficult to identify.
- Social Isolation: Feeling misunderstood by others or having trouble engaging in social activities can compound feelings of loneliness.
To combat depression, consider integrating the following strategies into your routine:
- Seek Professional Support: Don’t hesitate to reach out to a mental health professional. Therapy can provide valuable coping mechanisms.
- Engage in Self-Care: Prioritizing rest, proper nutrition, and physical activity can help lift your mood.
- Build a Support Network: Surround yourself with friends and family who understand your journey and can provide emotional support.
Anxiety Disorders
In addition to depression, many individuals with diabetes also grapple with anxiety disorders. The unpredictability that sometimes accompanies diabetes—such as sudden fluctuations in blood sugar—can create a constant sense of worry. Anxiety might manifest as:
- Excessive Worry: Constantly dwelling on blood sugar levels and potential complications can be mentally exhausting.
- Panic Attacks: Feeling overwhelmed can lead to panic attacks, leaving you feeling fearful and out of control.
- Avoidance Behaviors: Some may start avoiding situations that might provoke anxiety, like social gatherings or exercise.
It’s vital to recognize these feelings and seek help. I’ve seen how my cousin transformed her life by learning mindfulness techniques to manage her anxiety better. She shared that focusing on her breath and being present helped reduce her feelings of panic significantly. To address anxiety, consider these approaches:
- Practice Mindfulness: Meditation or yoga can help center your thoughts and reduce overall stress.
- Limit Stimulants: Reducing caffeine and sugar can prevent spikes in anxiety symptoms.
- Join Support Groups: Engaging with others in similar situations can reduce feelings of isolation and provide practical coping strategies.
In conclusion, addressing mental health complications like depression and anxiety is just as important as managing your physical health in diabetes. By prioritizing your mental well-being, you can create a more balanced, fulfilling life. Remember, it’s okay to ask for help—you’re not alone on this journey.
You might also find this article helpful Weight Management: Tips for a Healthy Weight





