What do white blood cells do for your body
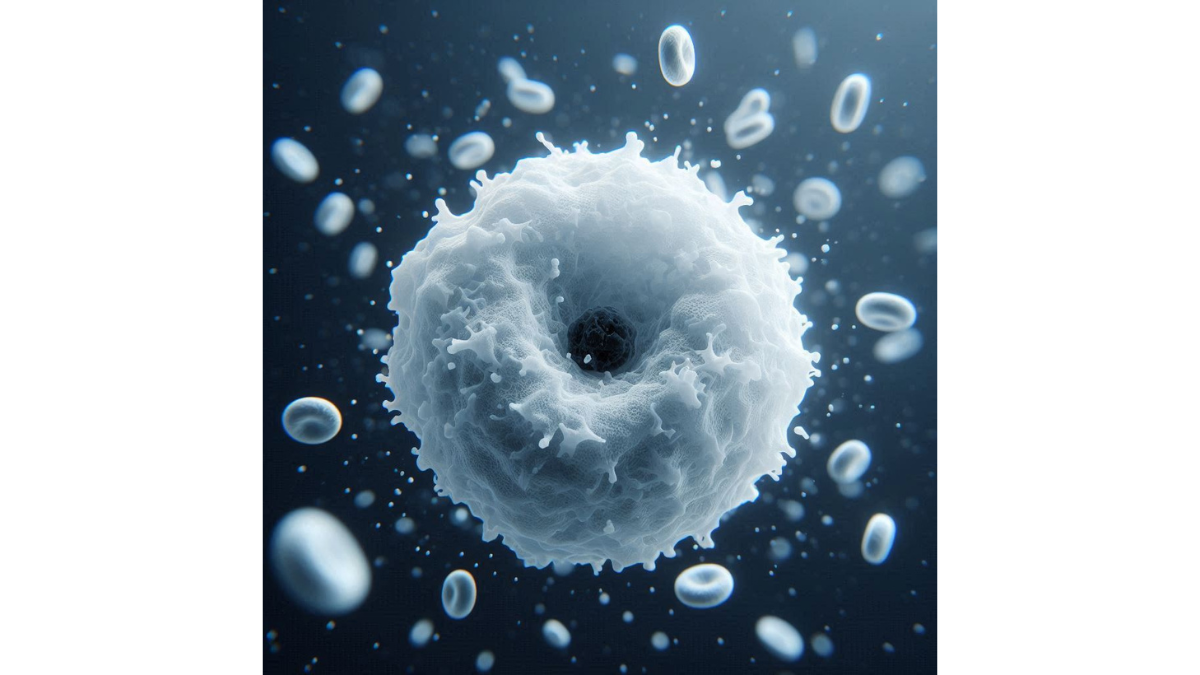
What do white blood cells do for your body – When considering the robust defense system of your body, white blood cells (WBCs) take center stage. These vital components of your immune system not only protect you from infections but also play a nuanced role in maintaining overall health. So, what exactly are white blood cells? In simple terms, they are the superheroes of your bloodstream, equipped to fight off pathogens and support bodily functions. There are several types of white blood cells, and each type serves a unique purpose. Here are the primary categories:
- Neutrophils: The most abundant type, neutrophils are often the first responders to infections, known for their ability to engulf bacteria and fungi through a process called phagocytosis.
- Lymphocytes: This subtype is crucial for adaptive immunity. It includes T-cells, which help regulate the immune response, and B-cells that produce antibodies targeting specific pathogens.
- Monocytes: These larger cells circulate in the blood and differentiate into macrophages and dendritic cells when they enter tissues. They are essential for both phagocytosis and antigen presentation.
- Eosinophils: Primarily involved in combating parasites and allergic reactions, these cells also help modulate inflammatory responses.
- Basophils: Though less common, basophils play a role in inflammatory reactions and are involved in allergic responses by releasing histamine.
These diverse types of white blood cells work in harmony to keep you safeguarded against a plethora of diseases. Understanding this provides insight into why boosting your immune health is crucial for maintaining wellness.
Importance of White Blood Cells in the Body
You may often hear about the importance of white blood cells, but how do they specifically contribute to your health? Their significance can hardly be overstated; they are involved in nearly every aspect of your immune response. To illustrate their indispensable role, let’s look at a few key contributions:
- Defense Against Infections: White blood cells are your body’s frontline soldiers, constantly on the lookout for invaders like bacteria, viruses, and fungi. When they detect an anomaly, they spring into action to neutralize the threat. It’s akin to having an alarm system that responds to intruders, ensuring your sanctuary remains protected.
- Healing and Repair: After combating an infection, white blood cells do not just retreat. They actively promote healing by clearing out dead cells and bacteria, paving the way for tissue regeneration. This is particularly vital after an injury when your body’s repair mechanisms are hard at work.
- Surveillance for Potential Health Problems: Beyond reacting to infections, certain white blood cells, such as natural killer (NK) cells, continuously monitor your body for abnormal cells, including those that could become cancerous. This surveillance mechanism serves as an essential check-and-balance system, helping to maintain your overall health.
- Memory Storage for Future Defense: Some lymphocytes have the remarkable ability to remember previous infections or vaccinations, enabling your immune system to respond more rapidly to pathogens upon subsequent encounters. It’s like your immune system keeps a list of previous ‘bad guys’ to recognize them instantly if they show up again.
heir various types cooperate through an ingenious network to tackle infections, facilitate healing, and keep a vigilant eye on your wellbeing. Knowing this can empower you to take steps to maintain or enhance your immune health, whether that means adopting healthier lifestyle habits or seeking medical advice when necessary. The next time someone questions “What do white blood cells do for your body?” you can confidently describe their essential roles in your immune defense system. From first responders to memory keepers, white blood cells are indeed your body’s unsung heroes.
Function of White Blood Cells
Immune Response
Building on the vital importance of white blood cells, let’s dive deeper into one of their primary roles: the immune response. Every day, your body faces countless threats from pathogens trying to invade and disrupt your health. White blood cells are your immune system’s backbone, specifically tailored to fend off these nuisances. When your body detects a threat, whether it’s a harmful bacterium or a pesky virus, it triggers a swift immune response. Here’s how it gets executed:
- Detection: The first step is the identification of the pathogen. This task is often led by macrophages, a type of white blood cell that patrols the body. They act like scouts, using receptors to sense foreign invaders.
- Communication: Once an intruder is detected, these cells signal to other types of white blood cells. This is where the beauty of teamwork shines through. They utilize molecules called cytokines to relay messages, amplifying the defensive alert throughout your immune system.
- Attack: Neutrophils are among the first responders in this battle. They rush to the site of infection to engulf and digest these pathogens through phagocytosis. Think of neutrophils as the frontline army digging trenches and strategizing attacks on the enemy.
- Coordination and Memory: After the invasion is quelled, T-cells and B-cells take the stage. B-cells produce specialized antibodies tailored to recognize and neutralize specific pathogens. In contrast, T-cells help regulate the immune response and destroy infected cells. The memory T-cells keep a digital file of these pathogens, a reminder for any future encounters.
Imagine a time you had a severe infection, like strep throat. That feeling of illness is typically due to your body battling the intruding bacteria. Throughout the process, white blood cells collaborated, ensuring that your immune system delivered a strong and coordinated response.
Inflammation and Healing
Now that we’ve navigated the complexities of the immune response, let’s explore another essential function of white blood cells: their role in inflammation and healing. It may sound counterintuitive, but inflammation, while uncomfortable, is a critical healing process set in motion by white blood cells. This involves several stages:
- Vasodilation: Blood vessels near the site of injury expand, increasing blood flow. This is why you might notice redness and warmth in the affected area. Increased blood flow means more immune cells and nutrients arrive on the scene.
- Recruitment of White Blood Cells: Neutrophils are typically the first responders to the site of inflammation. They travel through the bloodstream and migrate to the damaged tissue where they deploy their functions—engulfing pathogens and clearing debris. Following them, monocytes transform into macrophages to continue the cleanup and support healing.
- Healing and Tissue Repair: With the area clear of pathogens, the next step involves repairing the damaged tissue. Macrophages release growth factors that encourage the growth of new cells and the formation of new blood vessels. This process is akin to a construction crew clearing debris and building new structures where necessary.
It’s interesting to consider that inflammation is a double-edged sword. While it recruits necessary troops to fight off infections, it can also lead to discomfort and pain—think of a sprained ankle that swells up after you’ve rolled it on the basketball court. That’s inflammation working hard to protect you.
Production of White Blood Cells
Bone Marrow and Leukocytes
The story begins in the bone marrow, a spongy tissue found in the center of your bones, which serves as the manufacturing hub for all blood cells, including the vital white blood cells, or leukocytes. Bone marrow is a truly fascinating environment.Here’s a closer look at how white blood cells are created:
- Hematopoiesis: This is the process through which blood cells are formed. In the bone marrow, stem cells are stimulated to mature into different lineages of blood cells, including red blood cells, platelets, and, of course, leukocytes.
- Types of Leukocytes: The different types of white blood cells each have their developmental pathways. For instance:
- Granulocytes: Including neutrophils, eosinophils, and basophils, these cells all originate from the myeloid lineage.
- Lymphocytes: These consist of T-cells and B-cells, which are born from a separate lineage initiated within the bone marrow but complete their maturation in various lymphoid organs (like the thymus for T-cells).
Your body produces an enormous number of leukocytes daily. To illustrate, think of your bone marrow as a highly efficient factory, operating 24/7 to ensure that the defense mechanism in your body remains prepared. This production process is essential, especially during times of illness or injury, when your body may require an increased number of leukocytes to respond to an infection. Observing an increase in your white blood cell count is often a sign that your body is actively responding to a challenge.
Regulation of White Blood Cell Count
Maintaining the right balance of leukocytes is crucial for your immune system’s efficiency. If your count is too low, your body might be vulnerable to infections. Conversely, too many white blood cells could indicate an ongoing infection or even an autoimmune issue. Here are several factors that help regulate white blood cell production and count:
- Cytokines: These are signaling molecules produced by various cells in the body. They play a vital role in immune responses and influence the direction and quantity of white blood cell production. For instance, interleukins are a subset of cytokines that can stimulate the proliferation of specific white blood cells, while others can suppress cell production.
- Hormonal Regulation: Hormones, too, impact white blood cell counts. Specific hormones such as thymosin, produced by the thymus, promote T-cell maturation, while cortisol, a stress hormone, can suppress white blood cell production, leaving you potentially more susceptible to illness during stressful periods.
- Feedback Mechanisms: Your body has built-in feedback systems that monitor the levels of white blood cells.
- Lifestyle Factors: Your daily choices can influence white blood cell count as well. Diet, exercise, and sleep all play important roles. For example:
- Nutrition: A balanced diet rich in vitamins and minerals fosters optimal white blood cell health. Vitamins A, C, and E, along with minerals like zinc, contribute to maintaining a robust immune system.
- Exercise: Regular physical activity stimulates the production of immune cells and promotes better circulation.
- Stress: Chronic stress can lead to an imbalance in your body’s hormone levels and disrupt normal white blood cell production. Practicing mindfulness and relaxation techniques is beneficial.
Role of White Blood Cells in Fighting Infections
Phagocytosis
As we’ve delved into the intricate processes of white blood cell production and regulation, it’s essential to explore their frontline defense roles in fighting infections. Among the most critical functions of white blood cells is phagocytosis, a key mechanism through which these cells rid your body of harmful pathogens. So, how exactly does phagocytosis work? Think of it as a highly coordinated cleanup crew responding to an emergency. Here’s how the process unfolds:
- Recognition: When a pathogen, such as bacteria or viruses, enters your body, it’s often marked by specific molecules known as antigens. White blood cells like neutrophils and macrophages have receptors that can recognize these antigens, signaling them to inspect the intruder.
- Engulfing the Invader: Once recognized, the white blood cell extends its membrane around the pathogen, effectively engulfing it in a pocket known as a phagosome. This part of the process is reassuringly simple yet incredibly effective—the cell “sneaks up” on the pathogen and makes it its own.
- Destruction and Digestion: The phagosome then merges with a lysosome, which contains enzymes that break down the engulfed material. This is where the real magic happens: the enzymes dismantle the intruder, effectively digesting and neutralizing it.
- Waste Disposal: After the pathogen is dismantled, the remnants are expelled from the cell by exocytosis. This process ensures that only the debris is released while the white blood cell remains healthy and ready for the next challenge.
Antigen Presentation
Now that we’ve unpacked the process of phagocytosis, let’s move on to another vital role of white blood cells: antigen presentation. This process complements the actions of phagocytosis and is crucial for activating the adaptive immune response, which can offer long-lasting protection against specific pathogens. So, what does antigen presentation involve, and why is it significant?
- After Phagocytosis: When a macrophage or dendritic cell engulfs and breaks down a pathogen, it does more than just remove it. The cell processes the antigens—protein fragments derived from the pathogen—and displays them on its surface.
- MHC Molecules: The displayed antigens are shown on special receptors called Major Histocompatibility Complex (MHC) molecules. This is akin to a presenting board showcasing the “wanted” poster of an intruder to the immune system.
- Activation of T-cells: When a Helper T-cell encounters one of these antigen-presenting cells (APCs), it recognizes the presented antigen and binds to the MHC molecule. This binding acts as a signal, effectively activating the T-cell, which can now proliferate, differentiate, and launch a coordinated immune attack.
- Cytotoxic T-cells: They directly attack and kill infected cells displaying the same antigen.
- Helper T-cells: They play a crucial role in activating both B-cells and other immune cells.
- Long-term Immunity: This process not only addresses the immediate threat but also establishes memory cells that can swiftly respond to future infections by the same pathogen. This is why vaccines are effective—they prepare your immune system with a memory for specific antigens.
These mechanisms work seamlessly together, allowing your body to fend off intruders and build a robust immune memory.
White Blood Cells in Autoimmune Diseases
Relationship with Autoimmunity
Having discussed the vital roles of white blood cells in fighting infections and maintaining your health, it’s important to delve into a more complex and sometimes troubling aspect of their functionality: autoimmune diseases. Autoimmunity occurs when the immune system, instead of protecting your body, mistakenly targets its own cells, tissues, and organs. Understanding the relationship between white blood cells and autoimmunity is crucial in grasping the stages of these diseases. Here’s how:
- Misidentification of Self: Your immune system relies on a delicate balance of recognizing what is “self” and what is “non-self.” However, in autoimmune diseases, this distinction becomes blurred. White blood cells begin to identify normal, healthy cells as threats, launching an immune response against them. It’s as if your body’s alarm system starts reacting to familiar guests as intruders.
- Role of T-cells and B-cells: In many autoimmune conditions, T-cells and B-cells undergo abnormal activation. For instance:
- T-cells might mistakenly attack your body’s own tissues, leading to conditions like Type 1 Diabetes, where insulin-producing cells in the pancreas are destroyed.
- B-cells can produce autoantibodies that primarily target your own proteins, as seen in conditions like rheumatoid arthritis, where the joints become inflamed and painful.
- Inflammation and Damage: The constant activation of white blood cells results in sustained inflammation, which, over time, can lead to significant tissue damage.
She often shared stories of how small, everyday activities like walking in the park would turn painful due to her body’s own defense mechanisms misfiring. It can be heart-wrenching to see someone suffering from the very resilience designed to protect them. Understanding this harmful dysregulation of white blood cells can shed light on why autoimmune diseases can vary so dramatically in their symptoms and severity.
Treatment of Autoimmune Diseases Involving White Blood Cells
Now that we’ve established the unfortunate relationship between white blood cells and autoimmunity, let’s look at how we can manage these conditions. While there’s currently no cure for autoimmune diseases, treatment aims to minimize symptoms, induce remission, and stabilize the immune system. Here are some common approaches:
- Immunosuppressive Medications: These drugs are designed to dampen the immune response, limiting the activity of white blood cells. Some common medications include:
- Corticosteroids: These can quickly reduce inflammation and ease symptoms but must be used cautiously due to potential side effects with long-term use.
- Disease-modifying antirheumatic drugs (DMARDs): Often used in rheumatoid arthritis, DMARDs, like methotrexate, can help modify the body’s immune response in a more targeted manner.
- Biologics: A newer class of drugs that specifically target certain components of the immune system, biologics can halt the progression of autoimmune diseases. For example:
- TNF inhibitors block a protein that promotes inflammation, proving effective in conditions like rheumatoid arthritis and certain skin disorders.
- Lifestyle Modifications: Beyond medications, adopting lifestyle changes can also play a pivotal role in managing autoimmune diseases. This includes:
- Balanced Diet: Consume anti-inflammatory foods rich in omega-3 fatty acids, vegetables, and antioxidants.
- Regular Exercise: Engaging in physical activity can help improve overall health and reduce inflammation.
- Stress Management: Practicing relaxation techniques like yoga or meditation can lower stress levels, which is essential as stress can exacerbate autoimmune symptoms.
You might also find this article helpful Weight Management: Tips for a Healthy Weight





3 Comments