The Downside of Dental Implants: 5 Reasons to Reconsider
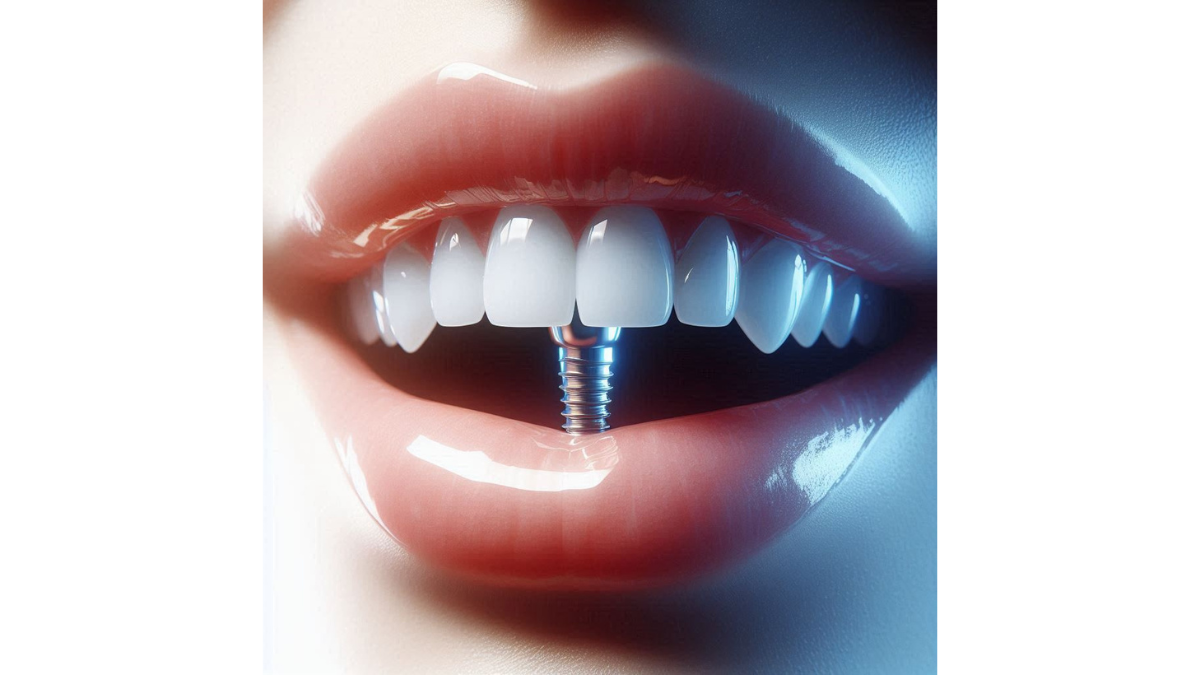
The Downside of Dental Implants: 5 Reasons to Reconsider – When it comes to dental health, the choices we make can have lasting effects on our well-being and confidence. One such option that has gained popularity in recent years is dental implants. While they promise a fixed and natural-looking solution for missing teeth, it’s essential to examine the flip side – the downsides of dental implants. It’s not uncommon for people to jump on the bandwagon without fully understanding the implications. Perhaps you’ve considered implants because they seem like an attractive option compared to dentures or bridges. However, before making a final decision, let’s take a closer look at some critical reasons to reconsider these seemingly ideal solutions.
Understanding the Landscape
The allure of dental implants often overshadows the challenges that accompany them. Many individuals have shared their stories about initial excitement turning into weeks of discomfort and unexpected costs. For instance, a friend of mine, Sarah, initially felt elated following her implant surgery but faced unexpected hurdles – both physically and financially. This experience, like many others, highlights the need for a thorough exploration of what dental implants entail.
A Deeper Dive into the Downsides
As we explore the downsides of dental implants, here are some critical areas of concern you should know:
- High Cost of Dental Implants:
- The initial investment can take a toll on your budget.
- Beyond the surgery, you must factor in additional expenses like follow-up care and potential need for bone grafting.
- Longer Treatment Process:
- The journey to a completed implant can stretch over several months, requiring multiple appointments and healing time that can feel tedious.
- Risk of Infection:
- Surgical site infections can arise post-operation.
- There’s also a risk of peri-implantitis, which could jeopardize your implant’s stability.
- Potential Complications:
- From nerve damage to sinus issues, complications can arise leading to more invasive treatments.
- Impact on Adjacent Teeth:
- The installation process can inadvertently affect neighboring teeth, leading to bone loss and even damage to these natural structures.
- Limited Longevity:
- While implants can last many years, wear and tear can necessitate replacements down the line, adding more costs.
Ultimately, understanding these downsides will empower you to make an informed choice about dental implants. It may seem like a simple fix, but acknowledging the potential pitfalls will better equip you for what lies ahead in your dental journey. Like any decision about your health, it requires careful consideration, balance, and clarity. As you weigh the pros and cons, let this guide serve as one step towards achieving a healthy smile that truly lasts. In the sections that follow, we’ll delve deeper into each of these aspects to paint a clearer picture of the downsides of dental implants and help guide your decision-making process. Get ready to approach your dental health with newfound awareness and insight!
High Cost of Dental Implants
As we’ve established, dental implants can be a life-changing option for those missing teeth. However, one of the most significant factors to consider is the high cost associated with this treatment. While the allure of a permanent, natural-looking smile might catch your attention, the financial implications can be daunting. Let’s break down the costs involved, starting with the initial investment.
Initial Investment
The first thing that might strike you is the initial investment required for dental implants. The costs can vary significantly based on several factors, such as location, the dental specialist’s experience, and the complexity of your individual case. On average, here’s what you might expect:
- Implant Fixtures: The implant fixture itself can cost anywhere from $1,000 to $3,000. This is the post that is surgically placed in your jawbone.
- Abutment and Crown: Once the implant is securely in place, you’ll need an abutment (a connector for the crown) and the crown itself, which can total an additional $1,500 to $3,000.
- Professional Fees: Don’t forget to factor in the dentist or oral surgeon’s fees, which can significantly add to the overall cost.
From my experience, when I was exploring dental implants for myself, the sticker shock of that initial estimate was quite overwhelming. I learned the hard way that “low-cost implants” might cut corners, leading to unsatisfactory results and higher costs later on if complications arise. It’s crucial to understand the full scope of investment before jumping in.
Additional Expenses
Beyond the initial investment, you’ll encounter various additional expenses that can catch you off guard. It’s essential to plan for these to avoid financial strain down the road. Here’s a list of potential extra costs:
- Diagnostic Imaging: Before surgery, you may need X-rays or 3D scans, which come with their fees. Expect anywhere from $100 to $500 for imaging.
- Bone Grafting: If your jawbone is insufficient to support an implant, you may require a bone graft, adding another $300 to $3,000 depending on the complexity.
- Follow-up Visits: Regular check-ups post-surgery are crucial for monitoring healing and ensuring implant stability. Each visit can cost between $100 and $300.
- Possible Additional Surgery: If complications arise, such as infections or issues with integration, you might face surgical costs again.
It’s essential to discuss all potential costs upfront with your dental provider to develop a comprehensive budget. By doing so, you’ll avoid unexpected bills that could dampen your journey to a confident smile. In conclusion, while dental implants can offer a permanent solution to tooth loss, the financial investment is significant and should not be overlooked. As we move ahead, let’s explore more complexities surrounding dental implants, particularly the longer treatment process that can also add to your overall commitment.
Longer Treatment Process
Having discussed the high costs associated with dental implants, it’s crucial to consider the treatment timeline. Many individuals overlook that the process of getting dental implants isn’t just a quick fix; it can take several months from start to finish. Understanding the timeline involved will help you set realistic expectations and prepare for what lies ahead.
Multiple Appointments
One of the most surprising aspects of the dental implant journey is the number of appointments needed throughout the process. It’s not just about making a single trip to the dentist; this is a multi-step affair. Here’s a quick breakdown of the typical appointments you might have:
- Initial Consultation: Your journey begins with a consultation, where the dentist assesses your oral health. This visit typically includes X-rays and discussions about your options.
- Treatment Planning: This appointment involves developing a detailed treatment plan based on your unique needs, which could take longer if additional procedures, like bone grafting, are necessary.
- Surgery: The actual implant placement requires a surgical appointment, usually lasting a couple of hours. After this, you’ll be sent home with post-operative care instructions.
- Follow-Up Visits: You’ll need several check-ups to monitor healing, assess the integration of the implant with your bone, and eventually fit you for the crown. These appointments can span several weeks or even months.
A personal anecdote that stands out for me is my friend Jason, who underwent this journey. He initially underestimated the number of visits required and ended up juggling his work schedule to accommodate the numerous appointments. It’s vital to factor in this aspect when planning your time.
Healing Time
While multiple appointments are necessary, healing time plays an equally crucial role in the overall treatment process. Healing time can vary depending on individual health, the complexity of the case, and whether other procedures were performed beforehand. Here’s a closer look:
- Osseointegration: This is the biological process where the implant fuses with your jawbone, and it can take anywhere from 3 to 6 months. During this period, you’ll need to adhere to specific dietary restrictions and avoid significant physical activity to aid the healing process.
- Soft Tissue Recovery: After the implant integrates with the bone, the surrounding gums must also heal adequately before the final crown can be placed. This process can take additional weeks.
- Temporary Solutions: While healing, some patients opt for temporary prosthetics to maintain their appearance. However, this solution can come with its own costs and challenges.
The extended healing time can be a test of patience, and it’s essential to keep your lifestyle and commitments in mind during this waiting period. As we transition into the next section, it’s vital to discuss the risk of infections that, though not common, can indeed add to the challenges associated with dental implants.
Risk of Infection
As we’ve navigated through the costs and the lengthy treatment process of dental implants, it’s essential to shed light on another significant concern: the risk of infection. While many people approach implant surgery with excitement for the potential restoration of their smiles, it’s critical to know that infections can complicate your journey. Let’s delve into two specific types: surgical site infections and peri-implantitis.
Surgical Site Infections
First and foremost, surgical site infections (SSIs) can occur after the initial implant placement surgery. Although dental implant surgeries are typically safe, there’s always a small risk that bacteria can infiltrate the surgical site. Here’s what you should know:
- Symptoms: After your implant surgery, be vigilant for signs of infection. Symptoms may include redness, swelling, warmth, and discharge at the surgical site. If you experience these, it’s essential to contact your dentist promptly.
- Causes: Various factors can contribute to SSIs, including poor oral hygiene, smoking, and underlying health conditions such as diabetes. For instance, a colleague of mine had a dental implant and, despite following the aftercare instructions, developed an infection due to uncontrolled diabetes. It was a tough lesson in understanding the importance of managing health conditions before surgery.
- Treatment: If an SSI occurs, your dentist may need to prescribe antibiotics or, in severe cases, perform additional surgery to clean the area. Thus, it’s vital to be proactive in keeping your mouth as clean as possible during recovery.
Peri-implantitis
Apart from SSIs, another threat is peri-implantitis, a condition that manifests as inflammation and infection of the tissues surrounding a dental implant. This can occur after the healing period and poses a long-term risk. Here’s a closer look:
- Symptoms: Similar to SSIs, signs of peri-implantitis include swelling, bleeding when brushing, and even loss of bone around the implant. If left untreated, it could lead to the loss of the implant itself.
- Prevention: Good oral hygiene practices are crucial in preventing peri-implantitis. Regular brushing, flossing, and using antimicrobial mouthwash can help keep your implants and gums healthy. Regular dental cleanings will also play a pivotal role in monitoring the health of your implants.
- Treatment Options: If peri-implantitis occurs, your dentist may recommend treatments ranging from deep cleaning around the implant to more advanced surgical options to restore health to the affected area.
Understanding these infection risks can seem daunting, yet awareness is a powerful tool to reduce your chances of complications. It reinforces the importance of maintaining excellent oral hygiene and attending regular check-ups. As we move forward, we will explore potential complications that can arise during or after the dental implant process, ensuring you are well-informed and prepared on your journey toward a new smile!
Potential Complications
Continuing our discussion about the challenges associated with dental implants, it’s important to address the potential complications that could arise during or after the procedure. While most patients achieve successful outcomes, there are risks that should not be ignored. Two significant complications to be aware of are nerve damage and sinus problems.
Nerve Damage
One of the more concerning risks of dental implant surgery is nerve damage. This complication typically occurs if the dental implant is placed too close to the nerves in the jaw. Understanding the implications of nerve damage is crucial:
- Symptoms: Nerve damage can result in sensations like tingling, numbness, or shooting pain in the area of the implant or radiating to other areas, such as the lips or tongue. If you experience these symptoms post-surgery, it’s essential to contact your dentist right away.
- Prevention: Dentists usually conduct thorough imaging studies, like X-rays or 3D scans, to map out the position of nerves before surgery. However, individual anatomical variations can sometimes make it challenging to avoid nerves entirely. It’s crucial to choose a qualified oral surgeon with experience in implant placements, as their expertise can significantly reduce the risk.
- A Personal Anecdote: A friend of mine had a dental implant placed and later experienced numbness in her lip. It turned out that the implant was positioned too closely to a nerve. Thankfully, her dentist intervened promptly, and although she required additional treatments, it highlighted the importance of open communication with your dental team about any post-operative sensations.
Sinus Problems
Another potential complication related to dental implants, particularly in the upper jaw, is sinus problems. If an implant is placed incorrectly or in a space that’s too close to the sinus cavity, complications can arise. Here’s what you need to know:
- Symptoms: Sinus complications can manifest as sinus pressure, congestion, or even persistent nasal discharge. Some patients might experience a feeling of something being lodged in their sinus cavities, which can be quite uncomfortable.
- Causes: The risk of sinus issues is particularly prevalent in procedures involving the upper molars and premolars, as the roots of these teeth are in close proximity to the sinus cavity. Therefore, careful planning and selection of implant type and placement is essential.
- Treatment: If a sinus problem arises due to an implant, your dentist might recommend a “sinus lift” procedure to reposition the implant or treat the sinus issue directly.
Awareness of these potential complications is essential in preparing for your dental implant journey. While the overall success rates are high, being informed and vigilant can help you navigate any bumps along the way. As we proceed further, we’ll discuss how dental implants can impact adjacent teeth, further underlining the need for thorough consideration before making a commitment.
Impact on Adjacent Teeth
As we continue to delve into the complexities surrounding dental implants, it’s crucial to consider how these procedures may affect your adjacent teeth. While implants can restore function and aesthetics to a smile, they can also pose risks to surrounding structures. In particular, two significant areas of concern are bone loss and damage to neighboring teeth.
Bone Loss
When a tooth is lost, the bone that once supported it begins to deteriorate over time. While dental implants are designed to reintegrate with your jawbone, the surrounding area can still be affected by the process. Here’s what you need to know:
- Bone Resorption: After losing a tooth, the jawbone begins to resorb, or break down, due to lack of stimulation. If an implant is not placed in a timely manner after tooth loss, significant bone loss can occur, making future implant placements more complicated.
- Impact on Adjacent Bone: When implants are placed, they should ideally prevent further bone loss. However, if the implant isn’t adequately sized or positioned, it can cause stress to the surrounding bone, leading to further bone resorption. This can result in complications if additional implants are needed later.
- Anecdote: I recall when my uncle lost a back tooth; he didn’t prioritize getting an implant until years later. When he finally did, the dentist discovered little bone where the tooth had been. My uncle faced additional bone grafting procedures, which prolonged treatment time and raised costs. It taught us both the value of addressing tooth loss promptly.
Damage to Surrounding Teeth
Another crucial consideration is the potential damage to adjacent teeth during and after the implant process. Here are some aspects to keep in mind:
- Preparation and Placement: The actual process of placing an implant requires a drill to be used on your jawbone to create space for the implant. If there’s not enough care taken, there’s a risk that surrounding teeth could be injured or loosened during this process, complicating an otherwise straightforward procedure.
- Misalignment: Implants that are improperly aligned can alter how teeth come together when you bite, which may lead to uneven wear or strain on adjacent teeth. Over time, this can result in issues like tooth mobility or even the necessity of further dental work.
- Support Structures: When adjacent teeth are affected by the implant process, you may not only experience discomfort but also require additional treatments for those affected teeth, leading to more expenses and time in the dental chair.
Recognizing the potential impacts on adjacent teeth emphasizes the importance of choosing a qualified professional to perform your dental implant procedure. Engaging with a skilled oral surgeon or dentist can help mitigate these risks through meticulous planning and execution. As we move toward a summary, it is essential to acknowledge that while dental implants offer many benefits, understanding the possible implications on adjacent teeth will help you make a well-informed decision regarding your oral health. In the next section, we’ll discuss the limited longevity of dental implants, rounding out our insights into this significant dental procedure.
Limited Longevity
As we wrap up our exploration of dental implants, it’s important to address an often-overlooked aspect: their limited longevity. While dental implants are celebrated for their durability and natural appearance, it’s essential to recognize that they are not invincible. Over time, wear and tear, combined with the potential need for replacement, can affect their effectiveness and overall health.
Wear and Tear
Like any dental restoration, dental implants endure daily wear and tear as they fulfill their function of chewing, biting, and smiling. Here are some key points to consider regarding wear and tear:
- Material Fatigue: While implants are made of high-quality materials such as titanium, they are still subject to the daily pressures of biting and grinding. Over the years, this can lead to fatigue, discomfort, or even implant failure if not evaluated regularly.
- Oral Hygiene: Maintaining excellent oral hygiene is crucial for the longevity of your implants. Inadequate care can lead to plaque buildup and subsequent issues, contributing to the overall wear on the implant over time. You know how your toothbrush sometimes feels like it doesn’t quite do the job? Imagine that on an implant level, where that wear can lead to bigger issues!
- A Personal Experience: I had a family member who received dental implants and initially enjoyed the benefits immensely. However, after a few years, they noticed some discomfort. It turned out they were grinding their teeth at night, which led to overuse of the implants. A night guard became essential, highlighting how everyday habits can affect longevity.
Need for Replacement
Eventually, even the most resilient dental implants may require replacement. Understanding the reasons behind this can help manage expectations and prepare for future dental care.
- Crown Replacement: While the implant itself may last for many years, the crown (the visible part of the implant) typically has a shorter lifespan, often lasting about 10 to 15 years with proper maintenance. Regular check-ups will help ensure you stay ahead of any potential issues.
- Implant Failure: Though relatively rare, implants can fail due to factors like infection, improper placement, or overstress over time. If an implant fails, it may need to be removed, requiring a new implant procedure, bone grafting, or other interventions.
- Anecdote: A close friend of mine, who received her implants over a decade ago, found herself needing a replacement crown recently. She was surprised but relieved that her regular dental visits helped her catch the issue before it led to an implant failure. This reinforces how ongoing dental care and attention play vital roles in implant longevity.
In summary, while dental implants can provide a long-lasting solution to tooth loss, they are not maintenance-free. Understanding the factors of wear and tear and the possibility of needing replacements can help you navigate your dental care with a clearer view. As you ponder your options regarding dental implants, consider these insights to ensure you make an informed decision that aligns with your long-term oral health goals. By doing so, you’ll be better prepared for a journey of smiles that last and truly enhance your quality of life!
You might also find this article helpful Building a Strong Foundation :Balanced Diet Enhances Your Health






2 Comments