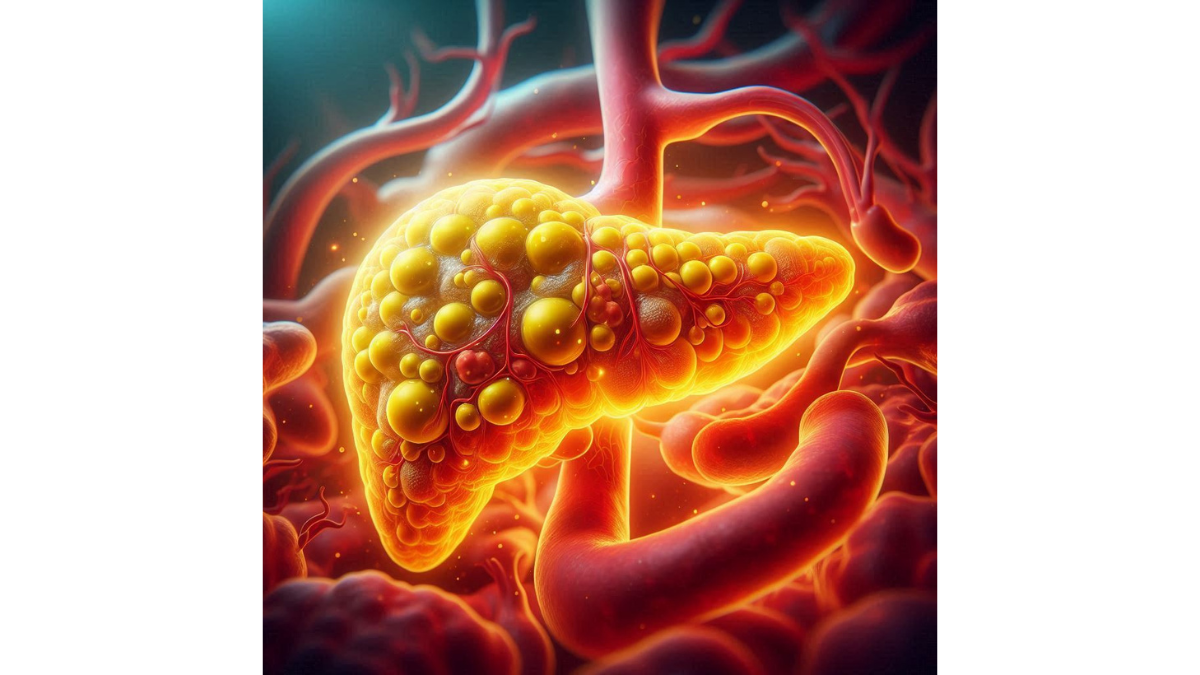
Gallstones: Causes Symptoms and Treatment Options – Gallstones are small, pebble-like substances that form in your gallbladder, which is a small organ located beneath your liver responsible for storing bile—a fluid that helps digest fats. When the ingredients of bile become imbalanced, it can lead to the formation of gallstones, which may vary in size from as small as a grain of sand to as large as a golf ball. You might wonder why they matter. For many, gallstones remain asymptomatic, meaning they don’t cause any noticeable issues. However, for some, these little troublemakers can lead to severe symptoms and complications. Picture this: you’re at a family gathering, enjoying your favorite meal, when suddenly you feel a sharp, gripping pain in your upper right abdomen—an indicator that gallstones could be at play. Gallstones can be categorized into two main types: cholesterol stones, which are the most common and typically yellow-green in color, and pigment stones, which are smaller and darker, made up of bilirubin.
How Common are Gallstones?
You might be surprised to learn just how prevalent gallstones are. According to various studies, nearly 10-15% of adults in North America have gallstones. That’s quite a substantial number! However, not everyone who has gallstones will develop symptoms or need treatment, making it a bit of a silent epidemic. Some key statistics that highlight the prevalence of gallstones include:
- Age: They are most common in people aged 40 and older.
- Gender: Women are more likely to develop gallstones than men, primarily due to hormonal factors.
- Family History: If someone in your family has gallstones, your chances of developing them may increase.
Interestingly, you might find that certain ethnic groups are more prone to gallstones. For instance, Native Americans and people of Hispanic descent tend to have higher rates. In summary, gallstones may seem like small, benign things, but they can disrupt daily life and lead to significant medical issues when they manifest. Understanding what gallstones are and how common they are is the first step in recognizing any symptoms you may experience and knowing when to seek medical attention.
Causes of Gallstones
Cholesterol Levels
When it comes to understanding the causes of gallstones, cholesterol levels play a significant role. You see, bile is designed to dissolve cholesterol, but when there’s too much cholesterol and not enough bile salts, your body struggles to keep everything in balance. This excess cholesterol can crystalize and form the infamous cholesterol gallstones. Picture this: you’re at dinner with friends, and you can’t resist the creamy Alfredo pasta or those crispy fried snacks. While treating yourself occasionally is perfectly fine, a diet high in saturated fats and cholesterol can elevate your cholesterol levels. This, in turn, increases your risk of developing gallstones. Here are a few key factors related to cholesterol levels that are important to consider:
- Dietary habits: High-fat diet, particularly those rich in animals fats, can lead to elevated cholesterol levels.
- Obesity: Being overweight contributes to increased cholesterol levels, making billions of plates of fried food call your name a little more loudly.
- Metabolic factors: Conditions like diabetes can also hinder the way cholesterol is processed in your body.
It’s essential to maintain a balanced diet to keep your cholesterol levels in check and mitigate the risk of gallstones.
Family History
Another significant contributing factor to gallstone development is family history. If you have a relative who has faced gallstones, there’s a chance that you might be more susceptible to them. Genetics can be quite influential, affecting everything from how your body processes cholesterol to the composition of bile. Think about it—have you noticed health patterns in your family? You might find gallstones on the family tree. Consider these points about family history and gallstones:
- Genetic predisposition: Certain genes can influence the likelihood of forming stones, meaning that if gallstones run in your family, your risk increases.
- Shared lifestyles: Often families share common dietary habits and lifestyle choices that can contribute to the risk of developing gallstones.
- Age and gender considerations: Since gallstones are more common in women and older adults, if these traits run in your family, the chances of developing gallstones may also rise.
In conclusion, while you may not be able to change your genetics, you can focus on maintaining a healthy diet and a balanced lifestyle to help mitigate the risk. Being mindful of cholesterol levels and understanding your family history can equip you with the tools to take proactive steps toward better gallbladder health.
Risk Factors for Gallstones
Gender
When it comes to the risk factors for gallstones, gender plays a remarkably significant role. Have you ever noticed how certain health issues seem to affect different genders differently? Well, gallstones are one of those conditions where women are particularly at risk. In fact, studies suggest that women are at least two to three times more likely to develop gallstones compared to men. Why is this the case? Hormones are to blame. Estrogen, for example, can increase cholesterol levels in bile and reduce gallbladder motility, meaning it doesn’t empty as effectively. This hormonal influence is why many women find themselves contending with gallstones, especially during pregnancy or while taking hormone replacement therapy. Here are some key points regarding gender as a risk factor:
- Pregnancy: Hormonal fluctuations during pregnancy can lead to slower gallbladder emptying.
- Hormonal therapy: Women who use oral contraceptives or hormone replacement therapy have a heightened risk.
- Age factor: Women become especially vulnerable post-menopause when hormonal changes occur.
Understanding these gender-related factors can help you take preventive measures and be more vigilant if you’re at a higher risk.
Obesity
Another significant risk factor closely associated with gallstones is obesity. If you find yourself struggling with extra pounds, you may be facing an increased likelihood of developing these pesky stones. Obesity affects the body’s processing and metabolism of cholesterol, which can lead to an overproduction of cholesterol in bile—a prime condition for stone formation. Imagine standing in front of the mirror and feeling frustrated with your weight. It’s not just about aesthetics; higher body weight elevates your risk for numerous health conditions, gallstones included. Consider these important aspects regarding obesity as a risk factor:
- Bile composition: Obesity can lead to an excess of cholesterol in bile, contributing to gallstone development.
- Gallbladder function: Being overweight can lead to decreased gallbladder motility, meaning your body isn’t efficiently processing bile.
- Dietary habits: People struggling with obesity often have dietary patterns that are high in fat and low in fiber—both of which can contribute to gallstone formation.
Combining awareness of gender susceptibility and the implications of obesity can empower you to make informed choices about your health. Whether incorporating more physical activity into your routine or adjusting your diet to include high-fiber foods, understanding these risk factors is crucial for prevention and overall well-being. Taking these proactive steps can go a long way towards reducing your risk of gallstones.
Symptoms of Gallstones
Abdominal Pain
When it comes to gallstones, one of the most common and distressing symptoms is abdominal pain. You might be familiar with that sudden, sharp pain that seems to take your breath away. It can occur in the upper right area of your abdomen or the center, radiating towards your back or right shoulder blade. This acute discomfort is known as a gallbladder attack or a biliary colic episode. Picture yourself at a lively family gathering, enjoying a delicious meal, when suddenly a sharp pain engulfs your abdomen. Juggling conversations with friends while simultaneously focusing on that stinging sensation can be quite overwhelming. Here are a few key characteristics of gallstone-related abdominal pain:
- Timing: The pain often occurs after eating a fatty meal, as your gallbladder works overtime to digest.
- Duration: This discomfort can last anywhere from 30 minutes to several hours.
- Resilience: The pain may come and go, making it challenging to pinpoint the exact cause or time of onset.
If you experience this kind of pain, it’s essential to pay attention and consider consulting a healthcare professional.
Nausea and Vomiting
In addition to abdominal pain, nausea and vomiting are common symptoms associated with gallstones. Imagine that same family gathering—one moment you’re laughing and enjoying dessert, and the next, waves of nausea crash over you, leaving you feeling weak and dizzy. The presence of gallstones can irritate your stomach and lead to a variety of gastrointestinal issues. Here’s what you should know about nausea and vomiting related to gallstones:
- Triggered by gallstones: These symptoms can arise from gallstones blocking the bile duct or gallbladder.
- Food impact: Fatty and heavy meals can exacerbate these feelings, making you wish you’d opted for a lighter dish.
- Severe cases: Persistent nausea may lead to vomiting, which can further complicate your overall well-being.
If these symptoms persist, becoming a frequent visitor, it’s always wise to consult a healthcare professional, as they can investigate the underlying causes. In conclusion, recognizing the symptoms of gallstones is crucial. Abdominal pain and nausea can act as red flags, warning you that it might be time to seek some medical advice. Being aware of these signs can empower you to take charge of your health and make informed decisions. So, next time something feels off, don’t hesitate to listen to your body!
Diagnosis of Gallstones
Ultrasound
When it comes to diagnosing gallstones, one of the most commonly used tools is an ultrasound. This non-invasive imaging technique has become a go-to method for healthcare professionals, and for good reason! It’s quick, painless, and doesn’t involve any radiation. Imagine lying comfortably on an examination table while a technician moves a small device over your abdomen, revealing images of your gallbladder on a screen. It may feel like a scene straight out of a medical drama! Ultrasounds work by using sound waves to create images of the organs within your body. Here’s how it helps in diagnosing gallstones:
- Direct Visualization: The ultrasound can show the presence of gallstones as well as any inflammation of the gallbladder.
- Monitor Size and Location: It allows doctors to see the size and location of any stones that may be blocking bile ducts.
- Quick Results: Typically, you’ll have results within a short timeframe, helping you get the answers you need quickly.
In fact, many people have described the ultrasound experience as surprisingly easy. Being proactive about your health means seeking a diagnosis early, especially if you’re experiencing symptoms like abdominal pain or nausea.
Blood Tests
In addition to ultrasound, blood tests play a crucial role in diagnosing gallstones and their potential complications. These tests can reveal important clues about your overall health and how well your gallbladder is functioning. You might picture yourself sitting in a clinic, chatting with the nurse while they draw blood from your arm—nothing to be overly concerned about. Here are some critical aspects regarding blood tests in the context of gallstone diagnosis:
- Liver Function Tests (LFTs): These blood tests measure enzymes and substances in your blood that indicate how well your liver and gallbladder are working. Elevated levels of certain enzymes could suggest a blockage in the bile duct.
- Complete Blood Count (CBC): This test helps identify any signs of infection, which is significant if complications like cholecystitis (inflammation of the gallbladder) occur.
- Bilirubin Levels: High bilirubin levels can indicate that your liver may not be functioning optimally, especially if gallstones are blocking the bile flow.
Taking these blood tests alongside an ultrasound provides a comprehensive view of not just whether gallstones are present, but also how they are affecting your health. If your doctor suspects complications, these tests can guide further treatment. In summary, being diagnosed with gallstones may sound daunting at first, but with tools like ultrasound and blood tests, securing an accurate diagnosis has never been easier. Getting the right information will empower you to take the necessary steps towards a healthier future. Don’t hesitate to reach out to your healthcare provider if you suspect gallstones—knowledge is power!
Complications of Gallstones
Pancreatitis
While gallstones can often be managed, they can also lead to serious complications if left untreated. One of the most concerning is pancreatitis, an inflammation of the pancreas that can occur when a gallstone blocks the pancreatic duct. Imagine going about your day, only to be suddenly struck by severe abdominal pain, which may radiate to the back—this is often a hallmark sign of pancreatitis. Here’s how pancreatitis connects to gallstones:
- Blockage: When a gallstone lodges in the pancreatic duct, it obstructs the flow of digestive enzymes, leading to inflammation.
- Acute vs. Chronic: Pancreatitis can be acute, leading to sudden and severe symptoms, or chronic, resulting from repeated episodes that cause long-term damage.
- Symptoms: Those suffering from pancreatitis typically experience intense abdominal pain, nausea, vomiting, and sometimes fever.
If you’re one of those people who have squeezed your way through an agonizing stomach ache or have felt nausea creeping in continuously, know that recognizing these signs can be life-saving. Early treatment is crucial to prevent the progression of pancreatitis, which can lead to further complications, including organ failure.
Cholecystitis
Another significant complication associated with gallstones is cholecystitis, or inflammation of the gallbladder. This condition occurs when a gallstone blocks the cystic duct, causing bile to accumulate and leading to gallbladder irritation and swelling. Picture it as a pressure cooker; when the pressure builds up inside, things can get messy! Here are some important aspects of cholecystitis:
- Symptoms: Common symptoms include intense pain in the right upper abdomen, fever, nausea, and vomiting. If you’ve experienced a combination of these, it might be time to consult a healthcare professional.
- Types: There are two types of cholecystitis—acute and chronic. Acute cholecystitis is a sudden inflammation, often requiring immediate medical intervention, while chronic cholecystitis is a recurring condition that can cause long-term damage.
- Treatment: If diagnosed, treatment may include fasting from food to allow your gallbladder to rest, as well as antibiotics to combat infection. In severe cases, surgical removal of the gallbladder (cholecystectomy) may be necessary.
In summary, while gallstones may seem like a minor issue at first, they can escalate into significant health complications like pancreatitis and cholecystitis. Recognizing the symptoms of these complications is vital for timely intervention, which can lead to better outcomes. Always prioritize your health, and take any alarming symptoms seriously by consulting your healthcare provider. Remember, prevention and timely action can make all the difference!
Treatment Options for Gallstones
Watchful Waiting
The journey towards treating gallstones doesn’t always begin with drastic measures. In fact, in many cases, doctors may recommend a strategy known as “watchful waiting.” This approach can be a valid option, especially for individuals who are asymptomatic or experiencing only mild symptoms. You might be asking yourself, “What does that even mean?” Simply put, watchful waiting involves monitoring the condition without immediate intervention. Imagine you’ve been feeling some discomfort but no severe pain or complications have arisen. Your doctor might suggest keeping an eye on your symptoms while maintaining a healthy lifestyle. Here’s why watchful waiting can be effective:
- Asymptomatic cases: If you’re not experiencing severe symptoms, it might be best to hold off on invasive treatments.
- Lifestyle adjustments: During this period, you can focus on dietary changes, such as reducing fat intake and increasing fiber-rich foods, which may help alleviate any discomfort.
- Regular check-ups: This approach allows you to maintain a dialogue with your healthcare provider and enables you to monitor any changes in your condition without being rushed into surgery.
Being proactive in your health while keeping a watchful eye on your symptoms can empower you to make informed decisions as you navigate your gallstone journey.
Surgery
However, if you find yourself dealing with recurrent gallbladder pain, complications, or significant symptoms that don’t improve, surgery may become a necessary consideration. The most common procedure for treating gallstones is a cholecystectomy, which involves the removal of the gallbladder. You may wonder about what to expect during this process. Here’s a breakdown:
- Types of Surgery:
- Laparoscopic Cholecystectomy: This minimally invasive procedure uses small incisions and is performed using a camera, allowing for quicker recovery times.
- Open Cholecystectomy: This traditional method involves a larger incision and may be necessary in more complicated cases.
- Recovery Time: Most people can resume regular activities within a week or two after laparoscopic surgery, though open surgery may require a longer recovery period.
- Post-surgery dietary adjustments: After gallbladder removal, individuals may need to adapt their diet. Avoiding high-fat meals for the first few weeks is often recommended to aid digestion.
In summary, the approach to treating gallstones can vary significantly from person to person. Watchful waiting offers a gentle approach for those with mild or no symptoms, while surgery may be necessary for individuals facing more severe complications. Ultimately, collaborating closely with your healthcare provider to determine the best treatment plan for you is the key to effectively managing gallstones. Remember, you’re not alone in this journey, and informed decisions can lead to better health outcomes!
Prevention of Gallstones
Dietary Changes
When it comes to preventing gallstones, making healthy dietary changes is a game-changer. Food plays a crucial role in shaping your body’s health, and being mindful of what you eat can significantly reduce your risk of developing gallstones. It’s easy to fall into the habit of indulging in rich, fatty foods, but a few strategic shifts can make all the difference. Consider this: Imagine replacing your usual buttery pancakes with a delicious bowl of oatmeal topped with fresh fruit. Not only does this forgo the excessive fats, but it packs in the fiber that supports digestive health. Here are some dietary changes to consider:
- Increase Fiber Intake: Incorporate more fruits, vegetables, and whole grains into your meals. Foods like beans, lentils, and oats can help keep your bile in check.
- Limit Saturated Fats: Cut back on fatty meats and dairy products. Instead, choose lean proteins like chicken, turkey, or plant-based options, along with healthy fats such as avocados and nuts.
- Stay Hydrated: Drinking plenty of water can help maintain proper bile consistency, reducing the likelihood of stone formation.
- Maintain a Balanced Diet: Focus on a well-rounded diet that includes a mix of macronutrients—carbs, protein, and fats—to keep your body functioning optimally.
It’s all about swapping processed snacks for nutritious options—a small change can lead to remarkable results!
Lifestyle Modifications
In addition to dietary changes, lifestyle modifications can play an equally important role in gallstone prevention. Think about the daily choices you make and how they all contribute to your overall health. Incorporating simple changes can help support your gallbladder while enhancing your well-being. Here are some lifestyle modifications to consider:
- Maintain a Healthy Weight: Achieving and sustaining a healthy weight can help regulate cholesterol levels and reduce gallstone risk. Slimming down gradually is key—rapid weight loss can actually increase the likelihood of stone formation.
- Stay Active: Regular physical activity is vital for a healthy gallbladder. Aim for at least 150 minutes of moderate exercise each week, such as brisk walking or cycling.
- Limit Sugar Intake: Reducing added sugars in your diet can help curb excess calorie consumption and maintain a healthy weight.
- Regular Health Check-ups: Engage in routine medical check-ups that include discussions about your diet, lifestyle, and any family history of gallstones.
In conclusion, prevention is often more manageable than treatment when it comes to gallstones. Implementing mindful dietary changes alongside positive lifestyle modifications can empower you to take control of your health. By focusing on what you eat and how you move your body, you set the stage for a healthier future. Remember, small changes can pave the way for significant improvements—embrace them!