Radiotherapy: its role in treating cancer – Radiotherapy is a medical treatment that utilizes high doses of radiation to kill or control the growth of cancerous cells. The primary goal of radiotherapy is to destroy malignant cells while minimizing damage to the surrounding healthy tissue. Imagine radiotherapy as a carefully targeted beam of light. Just as a laser can focus intensely on a single point, radiotherapy focuses radiation on the tumor, leaving much of the surrounding area unaffected. This precision makes it a critical component of cancer treatment. There are two main types of radiotherapy:
- External Beam Radiotherapy: This involves directing radiation from outside the body towards the cancerous cells.
- Brachytherapy: Here, radioactive material is placed inside or near the tumor, providing a more localized treatment.
Each of these methods plays a unique role in treatment plans based on the type and location of the cancer, and the patient’s overall health.
History of Radiotherapy
The journey of radiotherapy is both fascinating and transformative. The roots of this treatment date back to the late 19th century. In fact, the first medical application of radiation occurred shortly after the discovery of X-rays by Wilhelm Conrad Röntgen in 1895. By the early 1900s, doctors were starting to use radium and other radioactive materials in treatments. The first recorded use of radium in cancer therapy happened in 1903, marking a significant turning point in oncology. A few key milestones in the history of radiotherapy include:
- 1920s: Development of the first “Cobalt” machine, which allowed for statistical control over radiation doses.
- 1970s: Introduction of specialized equipment like linear accelerators (linacs), significantly improving targeting techniques.
- Today: Advanced methods such as Stereotactic Radiosurgery (SRS) have emerged, enabling precise treatment of tumors with minimal impact on neighboring tissue.
As technology has advanced, so too has our understanding of the mechanism of action of radiotherapy. Today, the focus is not only on destroying cancer cells but also on enhancing the patient’s quality of life during and after treatment. Radiotherapy’s evolution feels almost like watching a movie unfold, with each scene representing a crucial advancement in the battle against cancer. Through innovation and dedication, it has become a cornerstone in cancer treatment, providing hope to countless patients worldwide. With that understanding of what radiotherapy is and how it came to be, let’s delve deeper into the various types of radiotherapy next.
Types of Radiotherapy
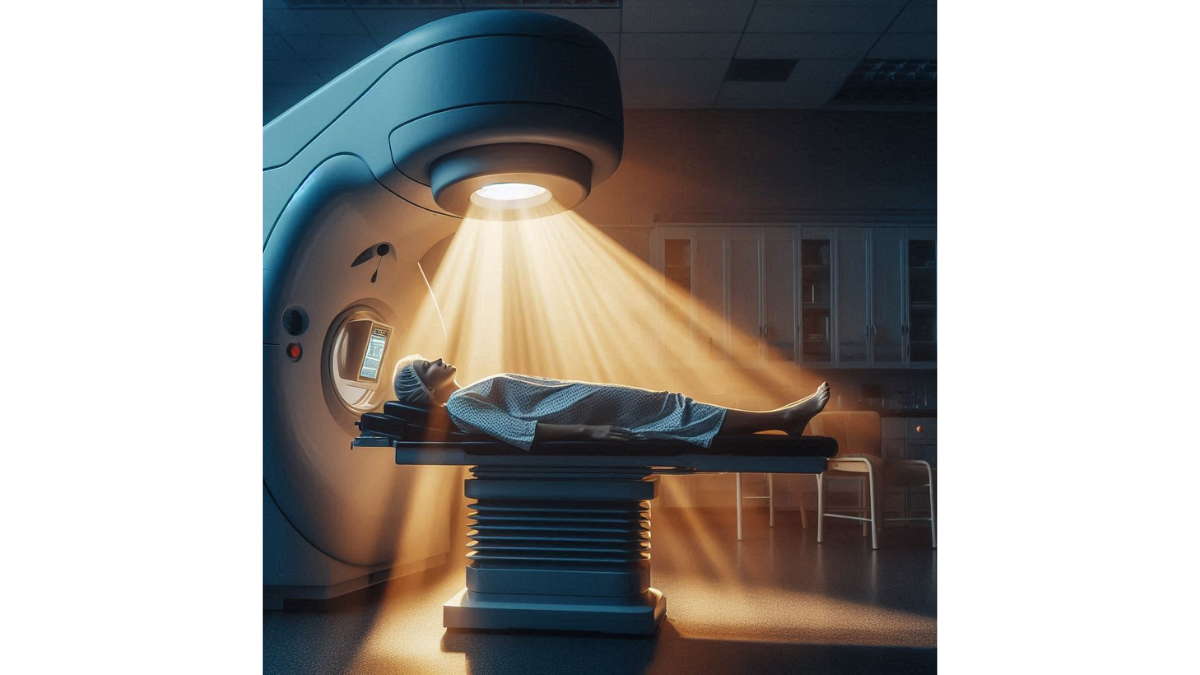
External Beam Radiotherapy
External Beam Radiotherapy (EBRT) is one of the most commonly used forms of radiotherapy. It involves directing a high-energy beam of radiation from outside the body onto the tumor site. Imagine standing outside on a sunny day, soaking up the sunlight; EBRT aims to deliver intense “sunlight” that targets only the cancer cells. The technique works through various advanced machines such as linear accelerators, which produce the high-energy beams of radiation. The treatment sessions typically last about 15 to 30 minutes and may be scheduled five days a week over several weeks. Here are several important points about EBRT:
- Precision: Modern imaging techniques like CT scans or MRI help to pinpoint the tumor’s location, ensuring that radiation is targeted where it is most needed.
- Variability: Different radiation techniques can be applied, including 3D-conformal radiation therapy, intensity-modulated radiation therapy (IMRT), and more.
- Sparing Healthy Tissue: Advanced methods help minimize the radiation exposure of nearby healthy cells, reducing potential side effects.
Many patients have shared their experiences regarding EBRT, often expressing relief at how quickly the sessions go by. One patient shared, “Honestly, while I was nervous before my first session, I soon found it became part of my routine—like going to get a haircut.”
Brachytherapy
Brachytherapy, on the other hand, takes a slightly different approach. This form of treatment involves placing radioactive material directly inside or very close to the tumor. Think of it like adding a sprinkle of seasoning directly onto a dish while cooking, making sure the flavor is concentrated right where it’s needed. Brachytherapy can be classified into two main types:
- Low-Dose Rate (LDR): Radioactive sources are implanted in the tumor, releasing radiation over a longer period.
- High-Dose Rate (HDR): This technique delivers a high dose of radiation at once, usually over a shorter time frame.
Benefits of Brachytherapy include:
- Localized Treatment: Greater concentration of radiation at the tumor site often leads to increased effectiveness.
- Shorter Treatment Times: Many patients can complete their treatment in a matter of days compared to weeks required for EBRT.
Personal stories often highlight the comfort of brachytherapy. A patient once remarked, “I was amazed at how little downtime I really had compared to what I expected. I was back to my normal activities almost immediately!” Understanding the differences between these two types of radiotherapy provides a clearer picture of how tailored cancer treatment can be. Next, let’s delve into the fascinating mechanisms that make radiotherapy effective in targeting cancer cells.
How Radiotherapy Works
Mechanism of Action
Radiotherapy operates on a fundamental principle: it damages the DNA of cancer cells, preventing them from multiplying and ultimately leading to their death. When you think about the intricate design of cellular structures, picture them as complex, sensitive machines—one small issue in a machine’s DNA can lead to a breakdown in function. This is precisely what radiotherapy aims to exploit. The radiation utilized in this treatment can take various forms, such as X-rays, gamma rays, or charged particles. The choice of radiation depends on factors like tumor type, location, and the overall treatment plan. Here’s how it works:
- DNA Damage: When radiation is absorbed by the tumor cells, it can directly affect their DNA or create free radicals—unstable molecules that indirectly damage the DNA.
- Cellular Response: Initially, cells may attempt to repair the DNA damage. However, the extent of that damage can result in misrepair, leading to cell death or malfunction.
- Apoptosis: If the damage is too severe, cells undergo a process called apoptosis (programmed cell death), effectively removing unhealthy or improperly functioning cells from the body.
Many patients are surprised by how targeted this treatment can be. One oncologist described it well: “Imagine every shot of radiation as a tiny sniper, carefully aiming at a cancer cell while trying its best to miss the healthy ones.”
Targeted Areas in the Body
Radiotherapy is not a one-size-fits-all treatment; its effectiveness relies on the precise targeting of specific areas in the body. While it can treat various forms of cancer, certain sites respond particularly well to radiotherapy. Here are some commonly targeted areas:
- Breast: Post-operative radiotherapy often targets remaining breast tissue and lymph nodes after surgery for breast cancer.
- Prostate: Radiotherapy can be an effective primary treatment or an adjunct after surgery for prostate cancer.
- Brain: Stereotactic radiosurgery, a form of EBRT, treats tumors in the brain with pinpoint accuracy.
- Lung: Radiotherapy can target lung tumors directly, especially in cases where surgery isn’t an option.
For example, one lung cancer survivor shared, “After my diagnosis, I was nervous about the treatment, but my team explained how they would target just the tumor. That made all the difference in my confidence.” Understanding how radiotherapy works and the areas it targets provides valuable insight into its role in cancer treatment. It’s remarkable how science has allowed us to develop such a refined and effective approach to combatting cancer. As we explore further, let’s look into the common side effects that patients might experience during this process.
Common Side Effects of Radiotherapy
Skin Reactions
One of the most noticeable side effects of radiotherapy is skin reactions. Because radiation is targeted externally, the skin in the treated area is often exposed to the rays, leading to various reactions. Picture the skin as a protective barrier; when it is bombarded with radiation, it may react similarly to a sunburn. Common skin reactions can include:
- Redness: This may appear as a mild blush on the skin, similar to what you’d experience after spending too long in the sun.
- Itching: Many patients report feelings of itchiness or irritation in the irradiated area.
- Dryness or Peeling: The skin may become dry and flaky, leading to peeling in more severe cases.
- Blistering: In some instances, blisters can develop, which require careful management.
It’s vital to have open discussions with your healthcare team about skin care during radiotherapy. For instance, one patient noted, “I was surprised by the way my skin reacted. My radiology nurse suggested creams to help soothe it, and that made a huge difference.” To manage skin reactions effectively, healthcare providers often give patients specific guidelines:
- Use gentle, fragrance-free soaps and lotions.
- Avoid tight clothing on the treated area.
- Protect the skin from sunlight exposure.
With diligent care, many patients find their skin reactions subside shortly after finishing radiotherapy.
Fatigue
Another common side effect of radiotherapy is fatigue. This isn’t just feeling a bit tired—it’s a profound sense of exhaustion that can affect your daily activities and emotional well-being. While it can vary in intensity from person to person, fatigue from radiotherapy can be surprising and sometimes overwhelming. The reasons for this fatigue can include:
- Body’s Healing Process: Your body expends energy to heal itself, which can lead to a feeling of tiredness.
- Impact on Blood Cells: Radiotherapy can also affect the bone marrow, resulting in lower blood cell counts, which can further contribute to fatigue.
Managing this fatigue involves listening to your body and pacing yourself. Some effective strategies might include:
- Short Rest Periods: Frequent, shorter breaks throughout the day can help keep energy levels manageable.
- Light Exercise: Gentle activities like walking or stretching can actually boost energy levels.
- Nutrition: Eating a balanced diet rich in vitamins and minerals supports overall health.
A patient reflected, “I learned to take naps and rest when my body told me to. It was hard at first, but it helped immensely.” Recognizing the common side effects of radiotherapy, such as skin reactions and fatigue, can help set realistic expectations for your treatment journey. This understanding will pave the way for better coping strategies as you navigate through this phase. Moving forward, let’s explore the advances in radiotherapy technology that are enhancing treatment outcomes and patient experiences.
Advances in Radiotherapy Technology
IMRT (Intensity-Modulated Radiation Therapy)
One of the most significant advancements in radiotherapy is Intensity-Modulated Radiation Therapy (IMRT). This cutting-edge technique provides a new layer of precision in radiation delivery, much like molding a light beam to fit perfectly around a detailed sculpture. With IMRT, radiation doses can be adjusted in intensity, allowing for a more tailored approach to treatment. This means that different parts of the tumor can receive varying levels of radiation based on their size and response to treatment. Here’s how it works:
- Modulation of Intensity: This is achieved by varying the strength of the radiation beams and using a series of adjustable collimators, which shape and direct the beams.
- Reduced Exposure to Healthy Tissue: Because of its precision, IMRT spares surrounding healthy tissue, leading to fewer side effects.
- Enhanced Targeting: Patients often feel more confident knowing their treatment is customized, akin to having a suit tailored just for them.
A breast cancer survivor shared, “With IMRT, I felt like my treatment was truly advanced. The doctors explained how it would focus on my tumor while protecting the healthy tissue around it.”
Stereotactic Radiosurgery
Stereotactic Radiosurgery (SRS) represents another incredible advancement in radiotherapy, particularly for treating tumors located in the brain. Despite its name, SRS is a non-surgical procedure that delivers high doses of radiation with pinpoint accuracy, much like a high-tech sniper targeting a specific area. Here are some key features of SRS:
- Single High Dose: Unlike traditional treatments that spread out the dose over several sessions, SRS typically administers a single, powerful dose of radiation.
- Precision Targeting: Advanced imaging techniques ensure that the radiation is directed precisely at the tumor, minimizing exposure to surrounding healthy brain tissue.
- Quick Treatment Time: Many patients can complete the procedure in a matter of hours, allowing them to return home the same day.
Patients find SRS reassuring, as one brain tumor survivor explained, “I was amazed at how quick and precise it was. It felt like being in a sci-fi movie, and knowing that I could go home the same day was a relief.” Advancements like IMRT and SRS are revolutionizing the field of radiotherapy, leading to improved outcomes and reduced side effects for patients. These technologies exemplify how innovative approaches are being adopted to make cancer treatment more effective and personalized. As we pivot to the next topic, let’s delve into how radiotherapy is increasingly being combined with other treatments to enhance overall effectiveness and patient outcomes.
Radiotherapy in Combination with Other Treatments
Chemoradiotherapy
Chemoradiotherapy, often referred to as chemoradiation, is a treatment that combines chemotherapy and radiotherapy. The idea here is simple yet powerful: by using chemotherapy to sensitize the tumor cells before radiation is applied, the overall effectiveness of cancer treatment can be significantly enhanced. Imagine facing a formidable opponent in a duel; if you have an ally by your side, your chances of winning increase dramatically. This is how chemoradiotherapy works: the chemotherapy drugs make cancer cells more vulnerable to radiation damage. Here are some key points about this approach:
- Synergistic Effects: Chemotherapy and radiation work together, allowing lower doses of each to be effective without overwhelming the patient.
- Improved Outcomes: Studies have shown that in certain cancers, such as head and neck, cervical, and lung cancer, combining these therapies can lead to better survival rates.
- Tailored Treatment: Oncologists can customize the treatment plan based on the cancer type, stage, and individual’s overall health.
A patient undergoing this dual treatment shared, “Initially, I was apprehensive about combining therapies, but my doctor explained how they would work together. It truly gave me hope.”
Immunotherapy
Another exciting frontier in cancer treatment is the combination of radiotherapy with immunotherapy. This strategy aims to harness the body’s immune system to fight cancer while using radiation to maximize the immune response. You can envision this as teaching an army how to fight battles while also deploying strategic artillery. The mechanics behind combining these therapies are intriguing:
- Stimulating Immune Response: Radiation can turn the tumor into an “inflammatory site,” attracting immune cells to the area. This, in turn, can help immunotherapy agents—like checkpoint inhibitors—work even more effectively.
- Targeting Metastasis: By using both therapies together, it may also be possible to target cancer cells that have spread to other parts of the body, increasing the chance of a comprehensive response.
- Personalized Approach: Not all patients will respond the same way, so treatments are often tailored, factoring in the unique characteristics of both the cancer and the patient.
One lung cancer survivor spoke of her experience: “After starting immunotherapy along with radiation, I noticed changes in my body I hadn’t expected. It felt like I was getting help from within myself.” The integration of chemoradiotherapy and immunotherapy with radiotherapy exemplifies how modern medicine is moving toward more comprehensive and personalized cancer treatment strategies. Through these combinations, patients are receiving enhanced care that addresses not just the tumor, but also the individual’s overall health. As we reflect on the collaborative nature of these treatments, let’s explore the vital role that radiotherapy plays in palliative care, focusing on pain management and symptom control for patients facing serious illness.
Radiotherapy in Palliative Care
Pain Management
Radiotherapy plays a pivotal role in palliative care, particularly in pain management for patients suffering from advanced cancer. While curative treatment may not be an option in these cases, radiotherapy can significantly improve the quality of life by alleviating pain and discomfort. Imagine having a persistent aching tooth: as long as the problem exists, it’s hard to concentrate on anything else. Similarly, pain can dominate a patient’s life when facing terminal illness. Here’s how radiotherapy helps:
- Targeting Painful Tumors: Radiation is effective in shrinking tumors that exert pressure on nerves or other structures, thereby reducing pain.
- Localized Treatment: With techniques like external beam radiotherapy, doctors can precisely target painful spots, delivering relief with minimal impact on surrounding tissue.
- Quick Onset of Relief: Many patients experience pain relief within days of receiving treatment, making it a timely option for those in distress.
A cancer patient undergoing palliative care shared, “The relief from pain after my radiotherapy sessions was amazing. It allowed me to enjoy moments with my family again.”
Symptom Control
In addition to pain management, radiotherapy is also essential for controlling various symptoms associated with advanced cancer. As cancer progresses, patients may encounter a range of distressing symptoms that impact their daily life. Radiotherapy can help address several of these challenges:
- Bleeding: For tumors in areas such as the head, neck, or pelvis, radiation can reduce tumor size and control bleeding.
- Obstruction: Radiotherapy can alleviate obstructions in the digestive tract or respiratory system caused by tumors, improving eating and breathing.
- General Comfort: The psychological relief gained from symptom management can significantly enhance a patient’s overall well-being.
One patient reflected, “I didn’t realize how much my symptoms were affecting my life until they started to improve after treatment. It was like a fog was lifted.” Incorporating radiotherapy into palliative care is a powerful approach that emphasizes comfort and support. It allows patients to focus on spending quality time with loved ones while managing the challenging symptoms they face. As we continue to explore the multifaceted role of radiotherapy, it’s important to note its critical contribution to overall cancer treatment strategies, offering hope and relief in complex situations. Now, let’s examine how radiotherapy plays a role in curative intent and its differentiation between adjuvant and neoadjuvant therapies.
Radiotherapy’s Role in Cancer Treatment
Curative Intent
Radiotherapy plays a critical role in cancer treatment with a curative intent. This means that the primary goal is to eliminate the cancer completely or significantly reduce its burden on the patient. Think of it as a determined effort in a team sport where the aim is to win the game—in this case, to eliminate the cancer. When radiotherapy is used with curative intent, it typically targets either localized tumors or areas where cancer may have spread. Here’s how it contributes to successful outcomes:
- Direct Tumor Targeting: By focusing radiation on the tumor, it destroys cancerous cells while sparing surrounding healthy tissue as much as possible.
- Combination with Other Treatments: Radiotherapy is often combined with surgery or chemotherapy to enhance effectiveness. For instance, many patients undergo surgery to remove the primary tumor followed by radiation to kill residual cancer cells.
- Higher Curative Rates: Studies show that when radiation is integrated into a treatment plan, particularly for cancers like breast, prostate, or cervical, the likelihood of complete remission increases.
One cancer survivor shared, “When I learned that my radiotherapy was part of a curative plan, it filled me with hope. I felt empowered knowing that we were actively fighting the cancer.”
Adjuvant vs. Neoadjuvant Radiotherapy
In the context of curative treatment, it’s essential to understand the differences between adjuvant and neoadjuvant radiotherapy. Both strategies utilize radiation, but they serve different purposes in the overall treatment plan.
- Adjuvant Radiotherapy: This refers to the use of radiation therapy after primary treatments like surgery. Its purpose is to eliminate any remaining cancer cells, reducing the risk of recurrence. For example, a patient might undergo surgery for breast cancer, followed by adjuvant radiotherapy to target any leftover microscopic disease.
- Neoadjuvant Radiotherapy: This approach uses radiation before the main treatment, typically surgery. The aim is to shrink the tumor to make it easier to remove or to preserve surrounding healthy tissue. An example would be a patient with esophageal cancer receiving neoadjuvant radiotherapy to reduce the tumor size and improve surgical outcomes.
These tailored approaches highlight the versatility of radiotherapy in cancer treatment, allowing healthcare teams to strategize effectively based on individual patient needs. A patient reflected, “Knowing there was a plan in place, whether it was before or after surgery, made me feel like I had a say in my treatment journey.” As we continue to navigate the evolving landscape of cancer treatment, it becomes clear that radiotherapy is not only a standalone treatment but also an integral partner in comprehensive cancer care. With advancements and personalized strategies, the future of radiotherapy continues to hold promise for improving patient outcomes.
You might also find this article helpful Happy Healthy and Whole : The Power of Positive Habits