targeted treatments for breast cancer
targeted treatments for breast cancer – When facing a breast cancer diagnosis, the overwhelming flood of information can sometimes leave you feeling adrift. Everything seems to move at lightning speed, from the initial appointment with your oncologist to the myriad treatment options available. However, one of the most hopeful developments in recent years has been the introduction of targeted treatments specifically tailored to treat breast cancer. Targeted treatments are designed to attack cancer cells while leaving normal cells unharmed, thereby minimizing side effects and improving outcomes. This approach represents a significant shift from traditional therapies like chemotherapy, which often affect both cancerous and healthy cells. Personal stories abound of patients who have benefited immensely from targeted therapies, and understanding these can empower your journey through treatment. Have you ever heard a friend mention how their sister had a successful battle against breast cancer? Perhaps that story involved a specific medication that targeted the cancer cells, showing how effective these advancements can be.
What Are Targeted Treatments?
At its core, targeted treatment involves drugs or other substances targeting specific characteristics of cancer cells. Instead of systemic approaches that affect the entire body, these therapies focus on fault lines in the cancer’s biological machinery. This can include prominent pathways involved in tumor growth or essential proteins that fuel cancer survival. A few key aspects to understand about targeted treatments include:
- Specificity: They hone in on unique markers of the cancer. For instance, some cancers have receptors that either promote or inhibit the growth of cancer cells.
- Reduced Side Effects: Because these treatments are more specific, you can expect potentially fewer side effects than traditional therapies.
- Tailored Approach: Your oncologist might recommend a targeted treatment based on your cancer’s characteristics, its behavior, and even genetic factors.
It’s essential to note that while targeted treatments can significantly improve outcomes, they aren’t suitable for every patient or every type of cancer. This is where comprehensive discussions with your healthcare team become crucial.
Personal Journey into Targeted Treatments
Take, for example, Laura, a 52-year-old mother of two, who discovered she had breast cancer after a routine mammogram. She recalls, “When I got the call, my world shattered. But when I learned about targeted therapy options, it felt like a glimmer of hope. The idea that there were treatments tailored just for my type of cancer gave me strength.” Laura’s experience highlights the emotional rollercoaster that comes with a cancer diagnosis. But the personalized nature of targeted treatments can provide reassurance, as they aim to address not only the cancer itself but also its unique biological fingerprint.
Categories of Targeted Treatments
For a legible understanding of how targeted treatments work, let’s categorize them into three main types:
- Hormone Therapy:
- Utilizes medications that slow or stop the growth of hormone-sensitive tumors.
- Commonly used for cancers that express hormone receptors.
- HER2-Targeted Therapy:
- Targets the HER2 protein, which promotes the growth of cancer cells in some breast cancers.
- This therapy blocks the HER2 pathway, effectively reducing cancer growth.
- Immunotherapy:
- Works by stimulating the immune system to fight cancer.
- This approach helps the body recognize and destroy cancer cells more efficiently.
The Future of Targeted Treatments
The landscape of breast cancer treatments is ever-evolving. As research progresses, more targeted therapies are becoming available, bringing hope to patients and their families. Clinical trials also play a vital role in this process. These trials are conducted to test new therapies, and participation can lead to access to cutting-edge treatments that might not yet be widely available. In summary, understanding breast cancer targeted treatments allows you to be more proactive in your health journey. Having informed discussions with your oncologist can lead to personalized treatment plans that align with your specific cancer type and individual preferences. By keeping informed and involved, you can better navigate the complexities of breast cancer treatment, equipped with the knowledge to make the best choices for your health and well-being.
Types of Targeted Treatments
As we delve deeper into the fascinating world of breast cancer targeted treatments, it becomes crucial to focus on the main types of therapies available today. With advances in medical science, you will find that treatments are becoming increasingly personalized. Here, we will explore two of the most prominent types of targeted therapies: hormone therapy and HER2-targeted therapy.
Hormone Therapy
Hormone therapy is a cornerstone of treatment for a specific subset of breast cancer, particularly those that are hormone-receptor-positive (HR+). This means that the cancer cells grow in response to hormones such as estrogen or progesterone. Understanding how hormone therapy works can provide you with a better perspective on managing your treatment.
How Does Hormone Therapy Work?
The primary goal of hormone therapy is to lower hormone levels in the body or block their action, thereby slowing or stopping the growth of hormone-sensitive tumors. Here’s how it usually works:
- Blocking Hormones: Medications may block the ability of hormones to promote cancer cell growth.
- Reducing Hormone Production: Other approaches reduce the body’s production of estrogen, effectively starving the cancer cells of the fuel they need to grow.
Typically, there are two classes of hormone therapies used in breast cancer treatment:
- Selective Estrogen Receptor Modulators (SERMs):
- Example: Tamoxifen
- How it works: These medications compete with estrogen for binding sites on the cancer cells. In simpler terms, they ‘block’ estrogen from doing its job, preventing cancer cells from growing.
- Aromatase Inhibitors:
- Examples: Anastrozole, Letrozole, Exemestane
- How it works: These drugs lower the estrogen levels in post-menopausal women by inhibiting the aromatase enzyme, which converts androgens into estrogens.
Personal Experience
Consider Sarah, a 45-year-old woman diagnosed with ER-positive breast cancer. During her treatment, she opted for hormone therapy. She recalls, “I was relieved to find out that my cancer was hormone-receptor-positive. The thought of taking a medication specifically designed to target my cancer felt empowering. Plus, I appreciated that it had fewer side effects than traditional chemotherapy.” Hormone therapy is particularly effective and often is a long-term strategy, potentially spanning five to ten years in many cases, offering continuous management of the disease.
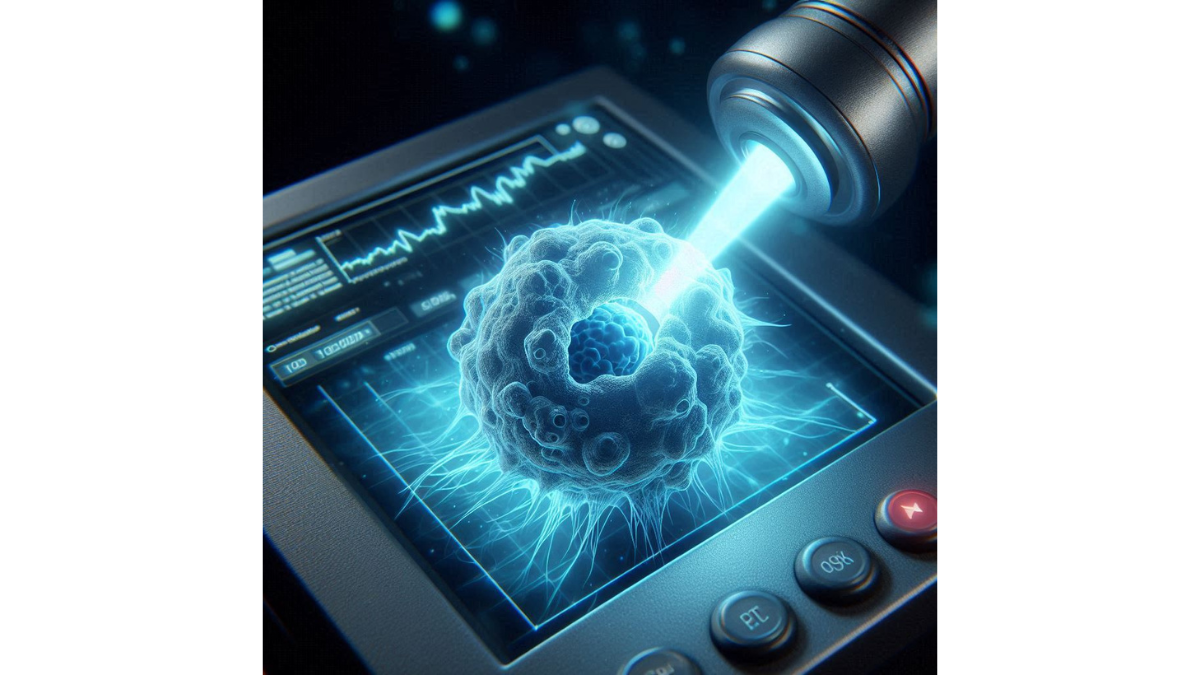
HER2-Targeted Therapy
HER2-targeted therapy is another significant advancement in breast cancer treatment, specifically targeting cancers that overexpress the human epidermal growth factor receptor 2 (HER2). This type is more aggressive and accounts for about 15-20% of breast cancers.
The Biology Behind HER2
To understand HER2-targeted therapy better, it’s essential to know what HER2 is:
- HER2 Protein: This protein plays a pivotal role in cell growth and division. When overexpressed, it leads to rapid cancer cell proliferation.
HER2-targeted therapies aim to hinder this pathway, effectively cutting off the cancer’s growth signals.
Types of HER2-Targeted Therapy
Some of the most common therapies include:
- Monoclonal Antibodies:
- Example: Trastuzumab (Herceptin)
- Use: It binds to the HER2 protein, blocking its signaling and marking cancer cells for destruction by the immune system.
- Tyrosine Kinase Inhibitors:
- Example: Lapatinib and Neratinib
- Use: These medications inhibit the signaling pathways activated by HER2, making it difficult for the cancer cells to grow.
Anecdote from a Survivor
Let’s look at Michelle’s journey, a 38-year-old breast cancer survivor. After being diagnosed with HER2-positive breast cancer, she started receiving trastuzumab as part of her treatment plan. “The moment I found out I had HER2-positive cancer, I was terrified. But once I started the targeted treatment, I felt optimistic. I knew that this was a specific approach to my cancer, and every appointment brought me a bit closer to recovery.” Michelle’s experience reinforces the notion that targeted therapies can transform potential fear into a sense of empowerment, giving patients like her a clear plan of action.
Conclusion
Both hormone therapy and HER2-targeted therapy are vital components in the fight against breast cancer. Their tailored approaches enable healthcare providers to develop treatment plans that cater to individual needs and cancer types. As you explore these options further, the journey becomes not just about treatment but about participating actively in your health decisions. Through understanding these technologies, you’re joining a community of informed patients and families striving for the best possible outcomes.
Targeted Therapy Drugs
Having discussed the types of targeted treatments available for breast cancer, it’s important to spotlight two of the most widely used and effective targeted therapy drugs: Tamoxifen and Trastuzumab. Each of these medications has unique mechanisms of action and specific applications that can significantly impact the course of treatment. Let’s delve into what makes these drugs so pivotal for many breast cancer patients.
Tamoxifen
Tamoxifen has long been a cornerstone in the treatment of HER-positive and hormone-receptor-positive breast cancers. As a selective estrogen receptor modulator (SERM), it works by interfering with the activity of estrogen in breast tissue.
How Tamoxifen Works
- Estrogen Receptor Blockade: Tamoxifen competes with estrogen to bind to its receptors on breast cancer cells, effectively blocking the hormone’s ability to promote cancer growth.
- Preventing Recurrence: Studies show that Tamoxifen is particularly effective at reducing the risk of recurrence in patients who have already been treated for early-stage breast cancer.
Who Should Take Tamoxifen?
Tamoxifen is typically prescribed for:
- Women with estrogen receptor-positive (ER-positive) breast cancer.
- Post-operative patients aiming to prevent cancer recurrence.
- Women at high risk of developing breast cancer, as it can also serve as a preventive measure.
Side Effects of Tamoxifen
While Tamoxifen is generally well-tolerated, side effects can occur. Some common ones include:
- Hot flashes
- Fatigue
- Mood swings
- Nausea
However, these side effects often decrease over time, and many patients find the benefits outweigh the discomfort. Take, for example, Lisa’s story — a 50-year-old who began Tamoxifen after her surgery for ER-positive breast cancer. She recalls, “The hot flashes were tough to handle initially, but my oncologist assured me it was a normal response. Knowing it was working toward my recovery kept me focused and positive.”
Tamoxifen and Longevity
Tamoxifen typically is prescribed for five to ten years post-surgery. This duration allows for robust prevention against recurrence and could significantly alter survival rates. The impact of long-term Tamoxifen therapy has been a game-changer for many women, leading to increased quality of life and reduced anxiety about future diagnoses.
Trastuzumab
Trastuzumab, better known by its brand name Herceptin, represents a significant advancement specifically targeting HER2-positive breast cancer. As a monoclonal antibody, it specifically hampers the HER2 protein that drives the aggressive nature of some breast cancers.
Mechanism of Action
- Binding to HER2 Protein: Trastuzumab binds to the HER2 receptors on the surface of cancer cells, blocking the signals that promote their growth and survival.
- Immune System Engagement: In addition to blocking HER2 signaling, Trastuzumab also recruits the immune system to attack and destroy cancer cells.
Who Should Take Trastuzumab?
Trastuzumab is usually indicated for:
- Patients diagnosed with HER2-positive breast cancer, either early-stage or metastatic.
- Combination therapy: Often used alongside chemotherapy for a synergistic effect, enhancing the overall efficacy of treatment.
Side Effects of Trastuzumab
While Trastuzumab can be life-saving, it comes with its own set of potential side effects, including:
- Flu-like symptoms (fever, chills)
- Nausea
- Heart-related issues (particularly in patients with pre-existing heart conditions)
Knowing her diagnosis of HER2-positive breast cancer, Margot shared her experience: “I was apprehensive about taking Trastuzumab, especially since my doctor warned me about potential heart issues. But the support and monitoring I received made me feel secure. After all, I wanted to fight this tough cancer head-on.”
The Role of Trastuzumab in the Fight Against Breast Cancer
The introduction of Trastuzumab has made a drastic impact on survival rates for HER2-positive breast cancer patients, offering hope where there was once little. The ONCOLOGY study famously reported that the combination of Trastuzumab and chemotherapy improved overall survival rates significantly compared to chemotherapy alone.
Conclusion
Both Tamoxifen and Trastuzumab are monumental drugs in the landscape of breast cancer treatment. They provide targeted, effective treatment options tailored to the specific subtypes of breast cancer, empowering patients like you with the information and tools necessary to navigate your treatment journey more effectively. As new research continues to emerge and clinical trials evolve, these targeted therapies not only save lives but also contribute to a more personalized and humane approach to oncology, making the treatment experience less daunting and more hopeful. By sharing experiences, building knowledge, and remaining proactive, you can face your breast cancer treatment with confidence.
Immunotherapy in Breast Cancer Treatment
As we continue our exploration of advanced treatment options for breast cancer, it’s crucial to discuss the innovative role of immunotherapy. This relatively recent addition to cancer treatment regimens has revolutionized how we approach various cancer types, including breast cancer. Among the immunotherapies gaining attention, Keytruda (pembrolizumab) stands out as a powerful weapon in the fight against specific forms of breast cancer, particularly triple-negative breast cancer (TNBC).
What Is Keytruda?
Keytruda is a monoclonal antibody designed to inhibit the programmed cell death protein 1 (PD-1) pathway. By blocking this pathway, Keytruda helps to activate your immune system against cancer cells, allowing your body to recognize and destroy them more effectively. This mechanism is particularly beneficial for cancers that have previously found ways to evade the immune system.
How Does Keytruda Work?
Here’s a simplified breakdown of how Keytruda functions:
- Targeting PD-1: Cancer cells can exploit the PD-1 pathway to avoid detection by the immune system. When Keytruda binds to the PD-1 receptor on T-cells, it “releases the brakes” on the immune system.
- Immune Activation: By blocking PD-1, Keytruda allows your T-cells to remain active and better equipped to find and destroy cancer cells that express PD-L1, a protein often found on the surface of tumors.
This innovative approach aids in re-arming your immune system, turning it into a more formidable opponent against cancer.
Who Is an Ideal Candidate for Keytruda?
Keytruda has been particularly effective in patients with triple-negative breast cancer, especially those whose tumors express PD-L1. Ideal candidates typically include:
- Patients with Triple-Negative Breast Cancer (TNBC): This subtype lacks estrogen, progesterone, and HER2 receptors, making it more challenging to treat. Immunotherapy offers a new avenue.
- High-Pacing Tumors: If a tumor has a high mutation burden or expresses PD-L1, there’s an enhanced likelihood that Keytruda will be an effective treatment option.
How Is Keytruda Administered?
Keytruda is administered through an intravenous infusion, typically every three weeks. The treatment plan may vary based on the stage of cancer and whether it is used alone or in conjunction with chemotherapy or other therapies.
Important Note on Monitoring
Doctors will closely monitor your response to Keytruda throughout the treatment. Regular imaging and tests will be conducted to evaluate effectiveness and adjust treatment as needed.
Side Effects of Keytruda
Like all treatments, Keytruda comes with its potential side effects, though many patients tolerate it well. Common side effects include:
- Fatigue
- Rash
- Nausea
- Diarrhea
While these effects can be unsettling, it’s essential to remember the importance of discussing any concerns with your healthcare team.
A Personal Touch
Consider the story of Elena, a 42-year-old woman diagnosed with triple-negative breast cancer. “When I was diagnosed, I felt lost. Chemotherapy was my immediate option, but I wanted something more targeted. My oncologist mentioned Keytruda, and I felt an air of optimism,” she shares. Elena was enrolled in a clinical trial assessing Keytruda’s effectiveness alongside chemotherapy. “I was amazed at how much energy I had throughout treatment compared to traditional methods. While it’s still a challenging journey, I felt like my immune system was fighting alongside me.”
Keytruda in Clinical Trials
Keytruda has been at the center of numerous clinical trials, leading to its FDA approval for treating TNBC in combination with chemotherapy. Clinical trials are essential not just for innovative treatments like Keytruda but also for refining use cases and managing side effects. Here are some findings from recent studies:
- Keytruda has shown improved overall survival rates compared to standard treatment, making it an exciting option for many patients.
- Patients in trials reported higher rates of tumor reduction and longer-lasting responses.
Conclusion
Immunotherapy represents a promising frontier in breast cancer treatment, and Keytruda exemplifies this evolution in therapy. By leveraging your immune system’s natural ability to fight cancer, Keytruda offers a targeted approach that may lead to better results and a more manageable treatment experience for many patients, especially those battling challenging subtypes like TNBC. As you navigate your journey through breast cancer treatment, staying informed about options like immunotherapy can empower you to make choices aligned with your health goals. With supportive healthcare teams and advancements like Keytruda, you’re not just a patient but a partner in your fight against cancer, equipped with powerful tools and options. Keep asking questions, remain proactive, and know that you’re not alone on this journey.
Clinical Trials for Targeted Treatments
As we explore the landscape of breast cancer treatments, it becomes increasingly evident that clinical trials play a pivotal role in advancing medical research and improving patient outcomes. These trials are the backbone of our understanding of how targeted treatments function, paving the way for newer therapies that can better manage and even eradicate cancer.
Importance of Clinical Trials
Clinical trials serve as critical testing grounds for new drugs, therapies, and treatment methods. Their importance cannot be overstated, as they not only contribute to scientific knowledge but also offer patients potential access to cutting-edge treatments. Let’s delve into what makes clinical trials so vital for both healthcare providers and patients alike.
Advancements in Cancer Treatment
- Discovery of New Treatments: Clinical trials often serve as the first step toward discovering and validating new treatment options. For example, breakthroughs in targeted therapies like Tamoxifen and Keytruda were only made possible through rigorous clinical studies that established their effectiveness and safety.
- Innovative Approaches: They allow researchers to test novel ideas and therapies that could become standard practice. This is particularly important in the field of oncology, where innovation is crucial for addressing the various complexities of different cancer types.
Patient Access to New Therapeutics
One of the most significant benefits of participating in clinical trials is access to treatments that aren’t yet available to the general public. This can be especially important for patients dealing with advanced or aggressive cancers, such as triple-negative breast cancer.
- Participants may receive innovative therapies: This includes drugs that target specific cancer markers, which may not yet be accessible outside the trial settings.
Contributions to Medical Research
By participating in clinical trials, you also contribute to the broader body of medical knowledge. Each trial adds valuable data that can inform future therapies and treatment guidelines.
- Your experience helps shape future cancer care: Every patient’s response to treatment is a piece of the puzzle. Participating in a trial provides essential insights that can ultimately improve treatment protocols for all patients facing similar diagnoses.
Informed Consent and Ethical Standards
Before enrolling in a clinical trial, participants receive detailed information about the study’s purpose, procedures, risks, and potential benefits. The informed consent process ensures that you fully understand what you are signing up for, creating a collaborative relationship between you and your healthcare team.
- Transparency: This process is crucial as it promotes transparency, allowing patients to make informed choices about their treatment options.
Navigating the Decision to Participate
Participating in a clinical trial is a personal decision, and it’s essential to weigh the potential benefits against the risks involved. Consider the following:
- Discuss with Your Healthcare Team: Open a dialogue with your oncologist or healthcare provider. They can help you evaluate whether a clinical trial is appropriate for your specific circumstances.
- Assess Your Health Condition: Each trial has eligibility criteria, so assess how your health aligns with those requirements before deciding.
A Personal Journey
Take Mark, a 50-year-old man treated for breast cancer, who decided to participate in a clinical trial for a new HER2-targeted therapy. He said, “When I learned that I might be part of something groundbreaking, it ignited a spark in me. I felt like I was actively fighting, not just passively waiting for treatment. Although it was a bit nerve-wracking, knowing I was contributing to research gave me a deeper sense of purpose.” His story illustrates how participation goes beyond the individual; it contributes to the greater good of cancer care.
Risks and Considerations
While clinical trials offer numerous benefits, they come with inherent risks. Understanding these risks is vital:
- Uncertain Outcomes: New treatments are not guaranteed to be effective, and patients may experience unknown side effects.
- Time Commitment: Trials often involve multiple visits, tests, and assessments that can require a substantial commitment.
Conclusion
In summary, clinical trials are a cornerstone of advancing breast cancer treatments. They provide patients with access to innovative therapies while contributing to the evolution of medical knowledge. As you explore treatment options, remember that participating in a clinical trial is not only a personal decision but also a step toward advancing cancer care for all. Stay proactive, communicate openly with your healthcare team, and consider how you can be part of this critical journey in the fight against cancer. Your involvement could be the key that unlocks a new doorway for future patients.
You might also find this article helpful Happy Healthy and Whole : The Power of Positive Habits