The Importance of Early Detection for Chronic Kidney Disease

The Importance of Early Detection for Chronic Kidney Disease – Chronic Kidney Disease (CKD) is a condition that affects millions of people around the world, often without them even realizing it. This silent epidemic gradually impairs kidney function over time, leading to serious health complications if not detected early.
Definition of Chronic Kidney Disease
So, what exactly is Chronic Kidney Disease? CKD is a progressive loss of kidney function, which typically occurs in stages, spanning from mild impairment to complete kidney failure. Essentially, it means that your kidneys are no longer able to filter waste effectively from your blood, leading to an accumulation of toxins and imbalances in electrolytes. The National Kidney Foundation defines CKD as:
- Stage 1: Kidney damage with normal or increased glomerular filtration rate (GFR) ≥ 90 mL/min
- Stage 2: Mild decrease in GFR (60-89 mL/min)
- Stage 3: Moderate decrease in GFR (30-59 mL/min)
- Stage 4: Severe decrease in GFR (15-29 mL/min)
- Stage 5: Kidney failure (GFR < 15 mL/min), requiring dialysis or transplantation for survival.
Recognizing CKD early can drastically improve outcomes and manage symptoms effectively, which is why being aware of its prevalence is vital.
Statistics on CKD Prevalence
The statistics surrounding CKD are quite alarming. According to recent studies:
- Approximately 37 million adults in the United States alone are estimated to have CKD.
- The prevalence of this disease is rising, with the global estimated prevalence now around 13% of the adult population.
- In older adults—particularly those aged 65 and older—CKD prevalence can reach upwards of 50%.
As your community and family members may be affected by this disease, it’s essential to understand the risk factors. For example, conditions such as diabetes and high blood pressure are among the leading causes of CKD. A friend of mine recently shared her experience with CKD; at first, she brushed off her persistent fatigue and nausea, attributing it to her busy lifestyle. When she finally got tested, she was shocked to discover that she had early-stage CKD. Thankfully, she caught it in time, which allowed her to make necessary lifestyle changes to manage her condition effectively. By understanding what CKD is and recognizing its prevalence, you can empower yourself and others to seek early diagnosis and prevention measures. Remember, knowledge is your ally when confronting the complexities of health issues like chronic kidney disease.
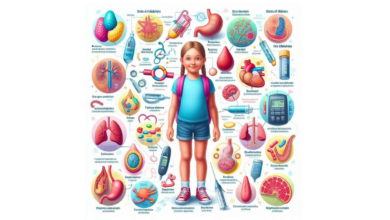
Early Warning Signs of CKD
Once you understand what Chronic Kidney Disease (CKD) is and its prevalence, it’s crucial to recognize the early warning signs. Early detection can lead to better management and outcomes, so keeping an eye out for symptoms can be life-changing.
Common Symptoms to Watch For
CKD often presents subtle symptoms that many people mistake for other health issues or simply aging. Here are some common indicators that may suggest kidney trouble:
- Fatigue and Weakness: Constantly feeling tired? This could be due to a buildup of toxins in your bloodstream, as your kidneys struggle to do their job.
- Swelling: Look out for swelling in your hands, feet, or face. This might indicate fluid retention, which occurs when your kidneys can’t properly remove excess fluid.
- Changes in Urination: Monitor your bathroom habits. Notice if you’re urinating more often, especially at night, or if your urine is foamy. Changes in color and consistency can also be red flags.
- Back Pain: While muscle strain can cause back pain, kidney-related discomfort is often felt in the lower back, just under the rib cage.
- Nausea and Appetite Loss: Persistent nausea and a reduced appetite can often be mistaken for something trivial, but they may indicate that waste products are accumulating in your body.
Sharing my own experience, I once dismissed my frequent bathroom trips as a result of drinking too much water. It wasn’t until I spoke with my doctor and underwent some tests that I realized it could signal something more serious.
Risk Factors for Developing CKD
Understanding the risk factors for CKD can help you be more vigilant about your health. Some common risk factors include:
- Diabetes: High blood sugar levels can damage kidney tissues over time. In fact, diabetes is the leading cause of CKD.
- Hypertension: Chronic high blood pressure can constrict blood vessels in the kidneys, leading to potential damage.
- Family History: If someone in your family has had kidney disease, you may be at higher risk.
- Older Age: The older you get, the higher your chance of developing kidney function decline.
- Cardiovascular Disease: Heart conditions can often intertwine with kidney problems.
- Obesity: It contributes to hypertension and diabetes, increasing your chances of CKD.
Being aware of these symptoms and risk factors can empower you to seek early testing through blood and urine tests and make lifestyle changes where necessary. Remember, timely action can make a tremendous difference in managing your health effectively.
Benefits of Early Detection
Recognizing the early signs of Chronic Kidney Disease (CKD) can have a profound impact on your health journey. Once you’ve identified the potential symptoms and risk factors, understanding the benefits of early detection becomes crucial.
Preventing Disease Progression
One of the most significant advantages of catching CKD early is the ability to prevent its progression to more severe stages. When detected in the initial stages, you can take proactive steps to slow down kidney damage, leading to a healthier, longer life. Here’s how:
- Lifestyle Modifications: Early detection allows you to adopt necessary lifestyle changes. These may include adopting a kidney-friendly diet, reducing salt intake, or managing stress, which can all contribute to healthier kidney function.
- Regular Monitoring: With an early diagnosis, you can establish a routine for regular monitoring through blood and urine tests. This diligent follow-up can catch any deterioration before it becomes critical.
- Catching Co-morbidities: Early detection often uncovers related health issues, such as diabetes or hypertension, allowing you to manage these conditions more effectively and protect your kidney health.
A good friend of mine was diagnosed with early-stage CKD a few years back. By understanding her condition early, she transformed her diet and began exercising, which has significantly slowed her disease progression.
Improving Treatment Outcomes
The second significant benefit of early CKD detection is the improvement of treatment outcomes. Here’s what you need to consider:
- Timely Medical Intervention: Early detection allows for timely medical intervention, which can include medications that specifically target the underlying causes of CKD, like high blood pressure or diabetes.
- Access to New Treatment Options: If CKD is caught early, patients can explore various treatment options rather than immediately relying on dialysis or transplantation. Options could include dietary supplements or specific medications aimed at preserving kidney function.
- Improved Quality of Life: Ultimately, early detection translates into a better quality of life. Patients can maintain their daily activities, enjoy their hobbies, and spend time with loved ones without the heavy burden of advanced kidney disease.
In essence, early detection of CKD equips you with the tools necessary to manage your health proactively. By acknowledging the symptoms, recognizing risk factors, and seeking regular check-ups, you become an active participant in your health journey. This not only leads to improved outcomes but gives you peace of mind as well, knowing you are taking charge of your well-being.
Screening Options for CKD
With the understanding of the benefits that come from early detection of Chronic Kidney Disease (CKD), it’s crucial to know the various screening options available. Regular check-ups and tests are key to monitoring kidney health, and fortunately, there are effective methods to assess your kidney function.
Blood and Urine Tests
The primary screening methods for CKD involve both blood and urine tests. These tests help provide a clear picture of how well your kidneys are functioning. Let’s break them down:
- Blood Tests:
- Serum Creatinine: This test measures the level of creatinine in your blood. Since creatinine is a waste product produced by muscles, elevated levels often indicate impaired kidney function.
- Glomerular Filtration Rate (GFR): Calculated from the serum creatinine level, GFR provides an estimate of how well your kidneys filter blood. A GFR of less than 60 mL/min can be indicative of kidney disease.
- Blood Urea Nitrogen (BUN): This test measures the amount of nitrogen in your blood that comes from urea, another waste product. High BUN levels can point to kidney dysfunction as well.
- Urine Tests:
- Urinalysis: This involves examining the content of your urine, checking for things like protein, blood, and other abnormalities that can signify kidney issues.
- 24-hour Urine Collection: This test measures how much urine your kidneys produce over a full day. It can provide insights into kidney function and electrolyte balance.
- Protein-to-Creatinine Ratio: An elevated protein level in your urine can signal kidney damage. This test compares the amount of protein to the amount of creatinine to assess kidney health.
When I was concerned about my own kidney health, I scheduled a routine check-up where these tests were conducted. Despite feeling completely fine, the results showed elevated creatinine levels, prompting further investigation. Early intervention allowed me to adapt my lifestyle quickly.
Imaging Studies for Kidney Function
In addition to blood and urine tests, imaging studies are essential tools for assessing kidney health. These non-invasive techniques provide a visual representation of your kidneys, often revealing underlying issues.
- Ultrasound: This method uses sound waves to create images of your kidneys. It can help detect abnormalities such as cysts, stones, or swelling that could affect kidney function.
- CT Scan: A computer tomography (CT) scan offers detailed images of the kidneys and surrounding structures, helping medical professionals identify potential problems more accurately.
- MRI: Magnetic resonance imaging (MRI) is another advanced technique used to visualize kidney structures and functions, often utilized when other imaging methods are inconclusive.
Utilizing combinations of these blood, urine, and imaging tests can provide a comprehensive view of your kidney health. Regular screenings should be part of your wellness routine, especially if you have risk factors for CKD. By staying proactive and informed, you empower yourself to take charge of your kidney health, allowing for timely interventions if necessary. Remember, early detection could make all the difference!
Lifestyle Changes to Manage CKD
Now that you have a clearer understanding of the testing options and the benefits of early detection for Chronic Kidney Disease (CKD), it’s time to explore the essential lifestyle changes that can help manage this condition. Two primary areas to focus on are dietary recommendations and the importance of regular exercise.
Dietary Recommendations for Kidney Health
Your diet plays a vital role in managing CKD and promoting kidney health. Making mindful choices can help reduce the workload on your kidneys and improve overall well-being. Here are some dietary recommendations to consider:
- Limit Sodium Intake: High sodium levels can lead to increased blood pressure and fluid retention. Aim to consume less than 2,300 mgof sodium per day.
- Tip: Use herbs and spices to flavor your meals instead of salt.
- Control Protein Consumption: While protein is essential for health, too much can strain the kidneys. Focus on quality over quantity. Choose lean protein sources like fish, poultry, and plant-based options.
- Watch Potassium and Phosphorus Levels: Depending on your stage of CKD, you might need to limit foods high in potassium (like bananas and avocados) and phosphorus (found in dairy products and dark sodas) to maintain a healthy balance.
- Stay Hydrated: Drinking enough water is crucial, but if you’re in advanced stages of CKD, your fluid intake may need to be restricted. Always consult your healthcare provider for personalized advice.
- Consult a Nutritionist: A registered dietitian can help you create a tailored meal plan that fits your lifestyle and health needs.
I remember when my dad was diagnosed with CKD; we worked together to revamp his meals. It was challenging at first, but finding kidney-friendly recipes turned out to be a fun and rewarding family activity!
Importance of Regular Exercise
Incorporating regular physical activity into your routine can significantly benefit your kidney health and overall quality of life. Exercise helps manage weight, lowers blood pressure, and improves cardiovascular health—all essential aspects to consider when living with CKD.
- Aim for a Balanced Routine: Combine aerobic exercises, strength training, and flexibility workouts into your weekly schedule.
- Examples of aerobic activities: Walking, swimming, or cycling for at least 150 minutes weekly.
- Strength Training: Resistance exercises using weights or resistance bands can build muscle and support bone health. Aim for at least two sessions per week.
- Stay Active Throughout the Day: Look for opportunities to move more: taking the stairs instead of using the elevator, gardening, or joining a local walking group.
- Listen to Your Body: Everyone’s fitness levels and limitations are different, especially with CKD. Always consult a healthcare professional before starting any new exercise regimen.
By adopting these dietary and exercise changes, you pave the way for better management of CKD. Remember, while it may feel daunting at first, small, consistent changes can lead to significant benefits over time. Prioritize your health, and celebrate every milestone along your journey!
Medication and Treatment Options
As you navigate the complexities of Chronic Kidney Disease (CKD), understanding your medication and treatment options is crucial. While lifestyle changes play an essential role in managing this condition, medications and more advanced treatments may be necessary to maintain kidney function and overall health.
Medications to Manage Symptoms
For many patients with CKD, medications are a vital part of their treatment plan to control symptoms and address underlying conditions. Here are some common types of medications that may be prescribed:
- Blood Pressure Medications: High blood pressure is both a cause and a consequence of CKD. Doctors often prescribe ACE inhibitors or ARBs (angiotensin receptor blockers) to manage blood pressure and protect kidney function.
- Diuretics: These help the kidneys remove excess fluid from your body, which can alleviate swelling and high blood pressure.
- Phosphate Binders: If your phosphate levels become elevated due to reduced kidney function, these medications can help prevent complications by reducing phosphate absorption from foods.
- Erythropoiesis-Stimulating Agents (ESAs): CKD can lead to a decrease in red blood cells. ESAs can stimulate your body to produce more red blood cells if you’ve developed anemia.
- Vitamin D Supplements: As kidney function declines, you may struggle to convert vitamin D into its active form. Supplements can support bone health and calcium regulation.
Taking medications can sometimes feel overwhelming. When my mother began her treatment journey, she had to manage several prescriptions. With the help of her doctor, we created a chart to visualize her schedule, which made it much easier to stay on track with her medications.
Dialysis and Transplantation as Treatment Options
As CKD progresses, some patients may ultimately require more intensive treatments, such as dialysis or kidney transplantation. Understanding these options can help you prepare for potential future needs.
- Dialysis: This is a treatment that performs the essential functions of healthy kidneys by removing waste, excess fluid, and harmful toxins from the blood. There are two main types:
- Hemodialysis: This typically occurs in a clinic three times a week, where a machine filters your blood.
- Peritoneal Dialysis: This method uses the lining of your abdomen to filter blood within the body, allowing for more flexibility and often can be done at home.
- Kidney Transplantation: When kidneys fail, a transplant from a donor can restore kidney function. This is often the preferred treatment for end-stage renal disease, as it can provide a more sustainable solution compared to dialysis.
Choosing between these options can be challenging, and it’s essential to work closely with your healthcare team to determine what’s best for you. I remember speaking with a neighbor who had undergone a kidney transplant; their experience was both inspiring and insightful, showcasing the transformative nature of this procedure. In conclusion, a comprehensive approach incorporating medications, potential dialysis, or even transplantation is vital for effectively managing CKD. By staying informed and connected with your healthcare team, you can navigate this journey with greater confidence and peace of mind.
Support and Resources for Patients
As you journey through the challenges of Chronic Kidney Disease (CKD), it’s essential to remember that you’re not alone. Support and resources are available to help you navigate both the physical and emotional aspects of this condition. Two critical areas to explore are counseling and mental health support, as well as financial assistance programs.
Counseling and Mental Health Support
Living with CKD can be both physically exhausting and emotionally draining. It’s completely normal to feel overwhelmed by this diagnosis, whether it’s managing symptoms or grappling with potential lifestyle changes. Seeking counseling and mental health support can provide the emotional resources necessary to cope effectively. Here’s how:
- Therapy Options: Individual therapy can help you process your feelings about your diagnosis, while group therapy offers the benefits of shared experiences and collective support. Connecting with others who understand what you’re going through can be tremendously reassuring.
- Stress Reduction Techniques: Many patients find that practicing mindfulness, meditation, or breathing exercises can reduce stress levels and improve emotional well-being. These techniques can serve as valuable tools to manage anxiety related to health concerns.
- Support Groups: Organizations like the National Kidney Foundation often host support groups where patients and caregivers can exchange experiences, tips, and emotional support. These communities can alleviate feelings of isolation and provide a sense of belonging.
A friend of mine, who has been living with CKD for several years, opened up about the relief she felt after joining a support group. She realized she wasn’t alone in her struggles, and the friendships she built there provided an extra layer of encouragement during tough times.
Financial Assistance Programs
Navigating the financial implications of CKD can be daunting. Treatment, medications, and regular check-ups can add up quickly, making financial assistance crucial for many patients. Here are some programs and resources to explore:
- Medicare and Medicaid: For eligible patients, these government programs help cover the costs associated with CKD, such as dialysis and kidney transplants. Be sure to check eligibility requirements and necessary documentation.
- Patient Assistance Programs: Many pharmaceutical companies offer programs to help cover the costs of medications. You can usually find these resources on their official websites.
- Nonprofits and Charities: Organizations like the National Kidney Foundation and the American Kidney Fund provide grants and assistance programs to help with medical expenses, transportation costs, and even utilities for patients facing financial hardships.
- Community Resources: Local community organizations may also offer financial assistance or connect you with services to ease your burden.
When my cousin faced a financial crisis during her treatment, she discovered a local charity that provided funds to cover her medical expenses. It showcased how vital community support can be in tough times. As you manage your health, don’t hesitate to seek support and explore the resources available to you. Whether it’s emotional care through counseling or financial assistance programs, every little bit helps in making your journey more manageable and less overwhelming. After all, your health and well-being should be your top priority, and you deserve to have the support you need.
Importance of Regular Monitoring
As we’ve explored the various facets of managing Chronic Kidney Disease (CKD), one essential aspect that cannot be overlooked is the importance of regular monitoring. Consistent check-ups and assessments not only enable early intervention but also enhance the overall management of the disease.
Role of Healthcare Providers in Disease Management
Healthcare providers play a critical role in the monitoring and management of CKD. Establishing a good relationship with your healthcare team can lead to better outcomes and a more personalized approach to care. Here’s how they contribute:
- Regular Assessments: Your healthcare provider will conduct regular blood and urine tests to monitor kidney function, track any progression of the disease, and adjust treatment plans accordingly. Discovering changes early can help slow the disease’s advance.
- Patient Education: Making sure you understand your condition is vital. Healthcare providers will explain your test results, risk factors, and provide resources that empower you to take charge of your health.
- Multidisciplinary Approach: CKD management often involves a team, including nephrologists, dietitians, social workers, and mental health professionals. This collaborative approach ensures that all aspects of your health are considered.
One of my family members was fortunate to have a nephrologist who emphasized patient education. She helped them understand kidney function, which instilled confidence in managing the condition. This foundation of knowledge also encouraged them to stay committed to regular check-ups.
Long-Term Prognosis for CKD Patients
The long-term prognosis for CKD patients varies significantly based on several factors such as the stage of the disease, underlying health conditions, lifestyle changes, and adherence to treatment plans. Here are some key points to consider:
- Disease Staging: The earlier CKD is diagnosed, the better the prognosis. Those diagnosed at Stage 1 or 2 often experience a slower progression compared to those diagnosed at Stage 4 or 5.
- Management Efforts: Keeping blood pressure, blood sugar, and cholesterol levels in check can have a profound impact on kidney health, lowering the risk of progression to end-stage renal disease.
- Lifestyle Modifications: Patients who make lifestyle changes—such as adopting a kidney-friendly diet, exercising regularly, and avoiding smoking—often see improved outcomes. Studies suggest that these changes can reduce the rate of kidney function decline significantly.
It’s important to remember that living with CKD doesn’t necessarily mean that you will face severe complications. Many patients successfully manage their condition for years, maintaining a good quality of life. In conclusion, regular monitoring is a cornerstone of managing CKD effectively. By staying engaged with your healthcare providers and understanding your long-term prognosis, you empower yourself to advocate for your health. This proactive approach can lead to better management of your condition, thereby enhancing your overall wellbeing and outlook on life.
You might also find this article helpful Weight Management: Tips for a Healthy Weight





4 Comments